Chapter: Introduction to Human Nutrition: Body Composition
Indirect methods - Body composition techniques
Indirect methods
Densitometry
The densitometric method assumes that the body consists of two components, a fat mass, in which all “chemical” fat is located, and the FFM, which consists of (fat-free) bones, muscles, water, and organs. Chemically, the FFM consists of water, minerals, protein, and a small amount of carbohydrate, the last often being neglected. The density of the fat mass is 0.900 kg/l and, from carcass analysis data, the density of the FFM can be calculated as 1.100 kg/l, depending on the relative amount of minerals, protein, and water in the FFM.
The density of the total body depends on the ratio of fat mass to FFM. Once the density of the body has been determined, the percentage of fat in the body (BF%) can be calculated by Siri’s formula:
BF% = (495/body density) − 450
Body density can be determined by several tech-niques, the oldest and perhaps most accurate being underwater weighing. Behnke first used the tech-nique, showing that excess body weight in American football players was not the result of excess fat but of enlarged muscle mass.
In underwater weighing, the weight of the subject is first measured in air and then while totally immersed in water. The difference between weight in air and weight under water is the upwards force, which equals the weight of the displaced water (Archimedes’ law), from which, after correction for the water tempera-ture (density), the displaced water volume (and thus the body volume) can be calculated. Corrections must be made for residual lung volume and air in the gut. Figure 2.1 shows an underwater weighing. The technique gives very reproducible results within about 1% of BF%. The absolute error in determined body
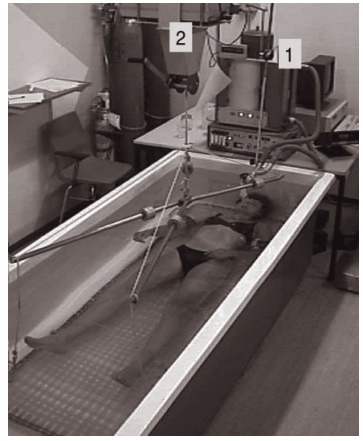
Figure 2.1 Underwater weighing. The subject is submerged com-pletely and breathes via a respirometer (1) for simultaneous residual lung volume measurement. Weight (W) (2) under water (uw) is recorded and density (D) is calculated as Dbody = Wair/(Wair − Wuw). Corrections are made for water temperature and lung volume: percent-age of fat in the body = 495/Dbody − 450.
fat is assumed to be maximal 3% of BF%. This error is mainly due to violation of the assumption that the density of the FFM equals 1.100 kg/l in the subject under study. It can be argued that in certain subjects or groups of subjects this assumption may be vio-lated, as for example in young children and in preg-nant women. Use of Siri’s formula will then lead to biased conclusions. Some laboratories have attempted to use water displacement instead of underwater weighing, but the technique failed, mainly because of the difficulty in accurately reading the water level in the tank.
An air-displacement method has been commer-cially available since 1995. This method measures body volume after placing the subject in a small, air-tight chamber and increasing the pressure by adding a known amount of air into the chamber. Boyle Gay-Lussac’s law enables the calculation of body volume. Corrections are made for temperature and humidity changes, and lung volume is assessed simultaneously.
Research to date has generally shown good agreement between underwater weighing and air displacement. Air displacement is better accepted by the volunteers, but some experience difficulties because of the breathing pattern to be followed or because of claustrophobia.
Dilution techniques
Carcass analyses revealed that the amount of water in the FFM is relatively constant at about 73%. Total body water (TBW) can be determined by dilution techniques. Dilution techniques are generally based on the equation:
C1 × V1 = C2 × V2 = Constant
where C is the tracer (deuterium oxide, tritium, or 18O water) concentration and V is the volume.
When a subject is given a known amount of a tracer (C1 × V1), which is known to be diluted in a given body compartment, the volume of that body com-partment can be calculated from the dose given and the concentration of the tracer in that compartment after equilibrium has been reached. Suitable tracers for the determination of TBW are deuterium oxide, tritium oxide, and 18O-labeled water. Other tracers can also be used, such as alcohol and urea, but they are less suitable because they are partly metabolized (alcohol) or because they are actively excreted from the body (urea) during the dilution period. After giving a subject the tracer and allowing around 3–5 hours for equal distribution throughout the body, determination of the concentration of deuterium in blood, saliva, or urine allows the calculation of TBW.
Alternatively, other tracers can be used, such as tritium oxide and 18O-labeled water, and the tracer can be given intravenously, which is advantageous when the subject has gastrointestinal disorders. The reproducibility of the method is 1–3%, depending on the tracer used and the analytical method chosen. From TBW, the FFM, and hence fat mass, can be calculated, assuming that 73% of the FFM is water:
BF% = 100 × (Weight − TBW/0.73)/Weight
The precision for estimations of body fat is about 3–4% of body weight. As with the densitometric method, this error is due to violations of the assump-tion used (i.e., that the relative amount of water in the FFM is constant and equals 73% of the FFM). In sub- jects with a larger than 73% water content in the FFM (pregnant women, morbid obese subjects, and patients with edema), the factor 0.73 will result in an overesti-mation of the FFM. A three-compartment model of the body that contains fat mass, water, and dry FFM has a lower bias than a two-compartment model. An overestimation of body fat by densitometry, for example because of a relatively high amount of water in the FFM, will be counteracted by an underestima-tion using the dilution method.
The use of tracers that do not cross the cell mem-brane enables the determination of extracellular water (ECW). Commonly used tracers in this respect are bromide salts or sodium-24. Intracellular water (ICW) cannot be determined directly and is calcu-lated as the difference between TBW and ECW.
Total body potassium
Chemical carcass analysis has revealed that the amount of potassium in the fat-free body is relatively con-stant, although the amount of potassium in different tissues varies widely. The determination of total body potassium (TBK) is relatively easy, owing to the natural occurrence of three potassium isotopes (39K, 40K, and 41K), in constant relative amounts, of which 40K is radioactive (gamma emission). Counting the emission of the gamma rays from the body reveals the amount of radioactive potassium, from which TBK and hence FFM can be calculated. The chamber in which the subject is scanned has to be carefully shielded to avoid any background radiation (cosmic radiation). The scanning of the body for potassium lasts for 20–30 min and the reproducibility is 2–3%.
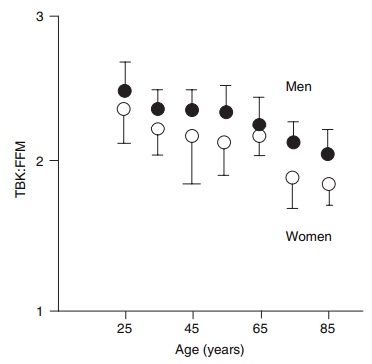
Several authors have shown that the amount of potassium in the FFM is different between males and females, is lower in obese subjects, and is probably also age dependent. Thus, TBK is much more useful as a measure of body cell mass (BCM) than as a measure of FFM. However, this discrepancy can be used to calculate the “quality” of FFM, defined as the ratio of cellular to extracellular components of FFM, or operationally as BCM/FFM. Thus, when TBK is used to assess BCM, and another method such as hydrodensitometry or DXA is used to assess FFM independently, it can be shown that the quality of FFM declines with age, along with the quantity (Figure 2.2). When potassium values are used to calculate intracellular water, BCM, or FFM, assuming constant amounts of potassium in these body components, the same errors can occur as with densitometry and dilu-tion techniques.
Although the technique is easy to apply in patients, the high cost of the scanning instrumentation limits its use other than in research settings.
Dual-energy X-ray absorptiometry
During DXA (also known as DEXA), the body or part of the body is scanned with X-rays of two distinct levels of energy. The attenuation of the tissues for the two different levels of radiation depends on its chemical composition and is detected by photocells.
The instrument’s software generates a two-dimensional picture of the body or the body compartment under study. The software can calculate several body com-ponents: bone mineral content and bone mineral density, lean mass, and adipose tissue fat mass. These calculations are possible for each of the body parts, e.g., for legs, trunk, spine, femur, and arms. However, the method cannot distinguish between subcutane-ous adipose tissue and discrete adipose tissue sites such as perirenal adipose tissue. The reproducibility of DXA is very high, varying from about 0.5% for bone mineral density to about 2% for total body com-position. The reproducibility for regional body com-position is less. The method is quick and easy to perform and places very few demands on the subject. The radiation dose (0.02 mSv) is only a fraction of the radiation dose of a normal chest radiograph, and hardly higher than the normal background. Apart from repeated scanning, the radiation dose should not be a limiting factor in terms of volunteers being exposed to hazardous levels of radiation. A disadvan-tage of the method is that the attenuation of the X-rays depends on the thickness of the tissue. Therefore, correction for the body size has to be made. Compared with traditional methods, DXA scanning is easy and widely available which, in turn, leads to prediction equations for body composition based on DXA. However, as with other methods, DXA relies on certain assumptions and there are many publications showing that the error in body composi-tion measurements using DXA can be considerable (Figure 2.3). Moreover, identical machines, even using the same software versions, can give different results in scanning the same person.
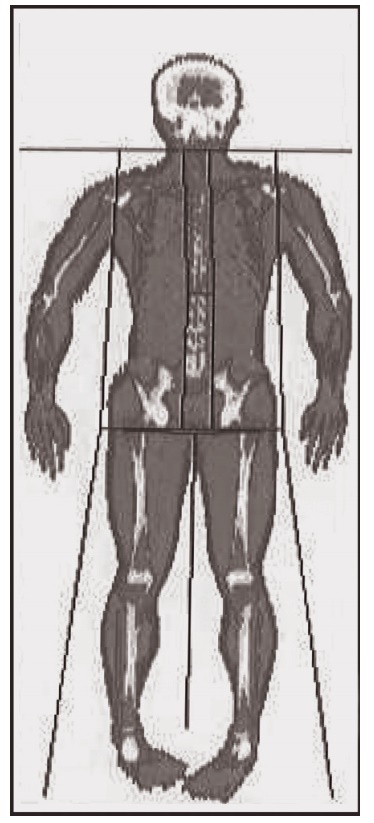
Figure 2.3 Dual-energy X-ray absorptiometer (DXA) scan using a HOLOGIC whole-body DXA (QDR-4500). Subcutaneous body fat, bone, and muscle are distinguished by different colors.
Multicompartment models
Two-compartment models, consisting of fat mass and FFM, lack validity in many situations where the composition of the body is “abnormal.” Examples already mentioned are pregnancy, morbid obesity, and the elderly. A combination of techniques often results in more valid estimates, as is the case when, for example, body density and body water are com-bined. In this particular case, the body is divided into three compartments:
Body weight = Fat mass + Body water + Dry fat-free mass
In this three-compartment model the variation of the water content in the FFM is accounted for. There are fewer assumptions in this model, leading to more valid results. Modern techniques such as DXA enable the valid and precise measurement of bone mineral, from which total body mineral can be estimated. When the mineral content of the body is com-bined with body density and body water, a four-compartment model of the body is generated:
Body weight = Fat mass + Water + Minerals + Protein
In this model, most of the variation in the amounts of the chemical components is accounted for, result-ing in a very reliable body composition measure. Four-compartment models can also be obtained using other techniques. For example, the measure-ment of calcium, phosphorus, and nitrogen with IVNAA in combination with TBW provides informa-tion for a model consisting of fat, minerals, protein, and water. In the literature, models based on six compartments are also described. However, they do not provide much additional information and the increased technical error negates the methodological advantage.
Imaging techniques
CT scanning enables the visualization of tissues in cross-sectional slices of the body. The thickness of those slices can vary, but is normally about 1 cm. During CT scanning a source of X-rays rotates per-pendicularly around the body or a body segment, while photodetectors, opposite to the source, register the attenuation of the X-rays after they have passed through the body in the various directions. The infor-mation received by the photodetectors is used to gen-erate images. Software enables the calculation of the
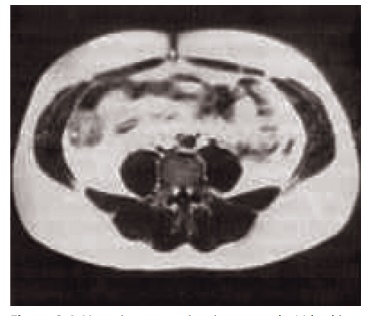
Figure 2.4 Magnetic resonance imaging scan at the L4 level in an obese subject. The white areas in the image are adipose tissue. Sub-cutaneous adipose tissue and intra-abdominal adipose tissue are sepa-rated by the abdominal muscles.
amounts of tissues with different attenuation, for example adipose tissue against nonadipose tissue. The CT technique was introduced for body composi-tion assessments in the 1980s and is now widely used, predominantly for measurements of body fat distri-bution. Figure 2.4 shows a scan of the abdomen at the level of the umbilicus, made by MRI, a technique that gives comparable information. The precision of the calculation of a tissue area or tissue volume from the same scan(s) is very accurate, with an error of about 1%. Partial volume effects (pixels that contain tissue with different attenuation) may influence the accu-racy and reproducibility of the method.
A single CT scan provides only relative data, for example in a scan of the abdomen the relative amount of visceral adipose tissue to subcutaneous adipose tissue. Multiple CT scanning allows the calculation of tissue volumes. From adipose tissue volumes (tissue level) and an assumed density and composition of the adipose tissue, the amount of fat mass (molecular level) can be calculated. Multiplying tissue volumes with specific densities of these tissues (determined in vitro) allows a recalculation of the body weight, a necessary but not sufficient exercise for validation of a whole body technique. Research in this area has shown that the CT technique allows the determina-tion of total body composition, with an error of estimate for fat mass of 3–3.5 kg (compared with densitometry).
CT scanning is expensive and, because of the rela-tively high level of radiation, the method is limited to subjects for whom scanning is indicated on clinical grounds. An alternative method to CT scanning is MRI, which has the advantage that no ionizing radia-tion is involved.
During MRI, the signals emitted when the body is placed in a strong magnetic field are collected and, as with CT scanning, the data are used to generate a visual cross-sectional slice of the body in a certain region. The determination of adipose tissue versus nonadipose tissue is based on the shorter relaxation time of adipose tissue than of other tissues that contain more protons or differ in resonance frequency. MRI has the advantage over CT scanning that the subject is not exposed to ionizing radiation. However, the time necessary to make an MRI image is relatively long (minutes versus seconds using CT), which has impli-cations for the quality of the image. Any movement of the subject, even the movements of the intestinal tract when making images in the abdominal region, will decrease the quality of the image.
As with CT scanning, images can be combined to obtain information on total body composition. Infor-mation about organ size can be obtained with a high accuracy. For example, MRI is used to study the con-tribution of various organs to the resting metabolic rate of the total body.
Both CT scanning and MRI are expensive, and therefore their use will remain limited to a few labo-ratories and for very specific situations.
Related Topics