Chapter: Basic & Clinical Pharmacology : Immunopharmacology
Immediate (Type I) Drug Allergy
IMMEDIATE (TYPE I) DRUG ALLERGY
Type
I (immediate) sensitivity allergy to certain drugs occurs when the drug, not
capable of inducing an immune response by itself, cova-lently links to a host
carrier protein (hapten). When this happens, the immune system detects the
drug-hapten conjugate as “modified self” and responds by generating IgE
antibodies specific for the drug-hapten. It is not known why some people mount
an IgE response to a drug, while others mount IgG responses. Under the
influence of IL-4, IL-5, and IL-13 secreted by TH2
cells, B cells specific for the drug secrete IgE antibody. The mechanism for
IgE-mediated immediate hypersensitivity is diagrammed in Figure 55–5.
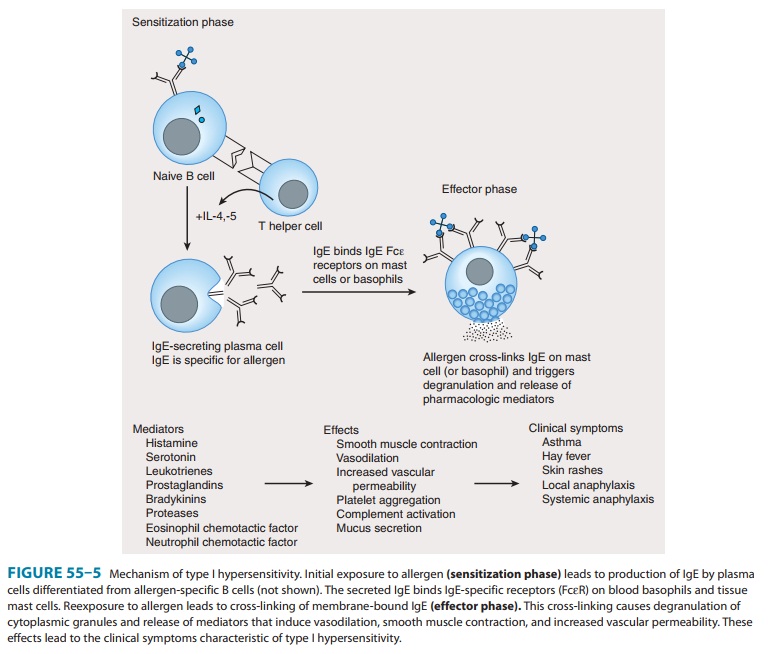
Fixation of the IgE
antibody to high-affinity Fc receptors (FcεRs) on blood basophils or their tissue
equivalent (mast cells) sets the stage for an acute allergic reaction. The most
important sites for mast cell distribution are skin, nasal epithelium, lung,
and gastrointestinal tract. When the offending drug is reintroduced into the
body, it binds and cross-links basophil and mast cell-surface IgE to signal
release of the mediators (eg, histamine, leu-kotrienes;) from granules.
Mediator release is associated with calcium influx and a fall in intracellular
cAMP within the mast cell. Many of the drugs that block media-tor release
appear to act through the cAMP mechanism (eg, cate-cholamines, glucocorticoids,
theophylline), others block histamine release, and still others block histamine
receptors. Other vasoac-tive substances such as kinins may also be generated
during hista-mine release. These mediators initiate immediate vascular smooth
muscle relaxation, increased vascular permeability, hypotension, edema, and
bronchoconstriction.
Drug Treatment of Immediate Allergy
One can test an
individual for possible sensitivity to a drug by a simple scratch test, ie, by
applying an extremely dilute solution of the drug to the skin and making a
scratch with the tip of a needle. If allergy is present, an immediate (within
10–15 minutes) wheal (edema) and flare (increased blood flow) will occur.
However, skin tests may be negative in spite of IgE hypersensitivity to a
hapten or to a metabolic product of the drug, especially if the patient is
taking steroids or antihistamines.
Drugs that modify
allergic responses act at several links in this chain of events. Prednisone,
often used in severe allergic reactions, is immunosuppressive; it blocks
proliferation of the IgE-producing clones and inhibits IL-4 production by T
helper cells in the IgE response, since glucocorticoids are generally toxic to
lymphocytes. In the efferent limb of the allergic response, isoproterenol,
epi-nephrine, and theophylline reduce the release of mediators from mast cells
and basophils and produce bronchodilation. Epinephrine opposes histamine; it
relaxes bronchiolar smooth muscle and con-tracts vascular muscle, relieving
both bronchospasm and hypoten-sion. The antihistamines competitively inhibit
histamine, which would otherwise produce bronchoconstriction and increased
cap-illary permeability in the end organ. Glucocorticoids may also act to
reduce tissue injury and edema in the inflamed tissue, as well as facilitating
the actions of catecholamines in cells that may have become refractory to
epinephrine or isoproterenol. Several agents directed toward the inhibition of
leukotrienes may be useful in acute allergic and inflammatory disorders .
Desensitization to Drugs
When reasonable
alternatives are not available, certain drugs (eg, penicillin, insulin) must be
used for life-threatening illnesses even in the presence of known allergic
sensitivity. In such cases, desen-sitization (also called hyposensitization)
can sometimes be accom-plished by starting with very small doses of the drug
and gradually increasing the dose over a period of hours to the full therapeutic
range . This practice is hazardous and must be performed under direct medical
supervision, as anaphylaxis may occur before desensitization has been achieved.
It is thought that slow and progressive administration of the drug gradually
binds all available IgE on mast cells, triggering a gradual release of
granules. Once all of the IgE on the mast cell surfaces has been bound and the
cells have been degranulated, therapeutic doses of the offend-ing drug may be
given with minimal further immune reaction. Therefore, a patient is only
desensitized during administration of the drug.
Related Topics