Structure, Viral Genes and Antigens, Pathogenesis, Clinical Features, Laboratory Diagnosis, Treatment - Human Immuno Deficiency Virus | 12th Microbiology : Chapter 10 : Medical Virology
Chapter: 12th Microbiology : Chapter 10 : Medical Virology
Human Immuno Deficiency Virus
Human Immuno Deficiency Virus
Human Immuno Deficiency Virus (HIV), the
etiological agent of AIDS, belongs
to the lentivirus subgroup of the family Retroviridae.
Infobits
Detecting HIV sooner
Fourth generation test helps to detect HIV in blood earlier than
previously recommended antibody test. It identifies the viral protein, HIV-1
P24 antigen, which appears in the blood sooner than antibodies.
Source: CDC
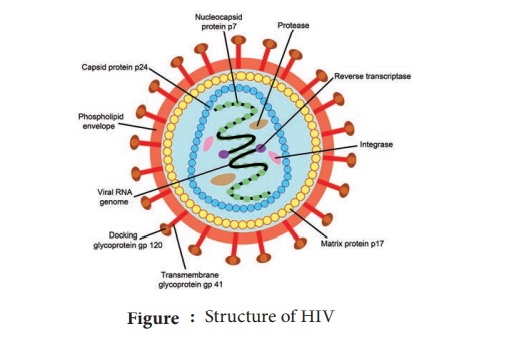
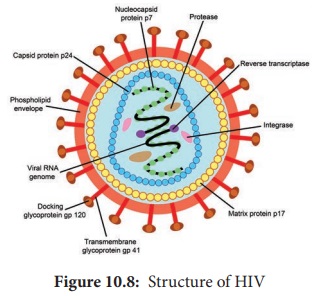
Structure
HIV is a
spherical enveloped Virus, about
90-120 nm in size. The nucleo capsid has an outer icosahedral shell and an
inner cone shaped core, enclosing the ribonucleo
proteins. The genome is diploid,
composed of two identical single
stranded, positive sense RNA copies. When the virus
infects a cell, the Viral RNA is
transcribed by the reverse transcriptase
enzyme, first into single stranded DNA and then to double stranded DNA
(provirus) which is integrated into the host cell chromosome. The virus coded envelope proteins are the projecting
knob like spikes which binds to the CD4 receptors on susceptible host cells
(Figure 10.8).
Viral Genes and Antigens
The
genome of HIV contains the three structural genes (gag, pol and env) as well as other nonstructural and
regulatory genes specific for the virus. These products of these genes, both
structural and non structural act as antigens.
Genes coding for structural proteins
1. The gag gene → Determines the core and shell of the Virus.
Precursor protein, p55 and it is cleaved into three proteins p15,
p18 and p24. Major
core antigen p24 can
be detected in serum
2. The env gene → Determines the syn-thesis of envelope glycoprotein
gp160. Cleaved in to gp120 and gp41
3. The
pol gene → Codes for the reverse
transcriptase and other viral
enzymes such as protease and
endonucleases. It’s expressed as a precursor protein, which is cleaved into
protein p31, p51 and p66.
Pathogenesis
Infection
is transmitted when the Virus enters the
blood or tissues of a person and comes into contact with a suitable host
cell, principally the CD4 lymphocyte. The receptor for the virus is the CD4
antigen and therefore the virus may infect any cell bearing the CD4 antigen on
the surface. Specific binding of the virus
to CD4 receptor is by the
envelope glycoprotein gp120.
Cell fusion is brought about by transmembrane
gp41. After fusion `with
the host cell membrane, the HIV genome is uncoated and internalized into the
cell. Viral reverse transcriptase mediate transcription of its RNA into double
stranded DNA, which is integrated into
the genome of the infected cell
through the action of the viral
enzyme integrase, causing a latent infection. The primary pathogenic mechanism
in HIV infection is the damage caused to the CD4+T lymphocyte. The T4 cells decrease is numbers. Infected T 4 cells do not
release normal amounts of interleukin, gamma interferon and other lymphokines,
this is damping effect on cell mediated immune response.
Clinical Features
AIDS is
only the last stage in the wide spectrum in HIV infection.
1. Acute HIV infection
3–6 weeks
of infection, persons experience low grade fever, malaise, headache,
lymphadenopathy, with rash. Antibodies are usually negative at the onset of the
illness but become positive during its course called ‘Sero conversion illness’.
2. Asymptomatic or latent infection
All HIV
infected persons, whether or not they experience Sero conversion illness, pass
through a phase of symptomless infection
which may last up to several years.
The infection progresses in course of time through various stages, CD4
lymphocytopenia, minor opportunistic infections, AIDS-related complex (ARC),
ultimately terminating to AIDS.
3. Persistent
generalized lymphadenopathy (PGL)
It is
defined as the presence of enlarged lymph nodes at least 1cm, in diameter
in two or more non contiguous
extrainguinal, sites that persists for at least three months.
4. AIDS related complex (ARC)
This group includes patients with considerable immunodeficiency, suffering from
various symptoms or minor opportunistic infections. eg. Oral candidiasis,
Salmonellosis or Tuberculosis.
5. AIDS
End-stage
disease, poor immune defence mechanism leading to the opportunistic infection
and malignancies.
a. Commonest symptoms
Drycough,
dyspnea and fever. Pheumonia may be viral (cmv) or fungal (Cryptococcus,
Histoplasma).
b. Gastrointestinal system
The mouth
is often involved with thrush, stomatitis, gingivitis, hairy leukoplakia.
Dysphagia due to esophageal Candidiasis. Intestinal pathogen in AIDS is
cryptosporidium. Other pathogens are Salmonellae, Mycobacteria, CMV or adeno
viruses. Gay bowel syndrome’ is common among the male homosexuals.
c. Central nervous system
The
typical CNS opportunistic infections are toxoplasmosis and cryptococcosis.
Lymphomas of the CNS are Common.
d. Malignancies
Kaposi’s
Sarcoma was the lesion seen in male homosexuals. The tumours commonly seen are
lymphomas, both the Hodgkin and non Hodgkin types.
e. Cutaneous
Herpes
lesions, Candidiasis, Dermatitis, impetigo are common cutaneous lesions.
6. Dementia
Direct cytopathogenic damage in the CNS. It
cross the blood-brain barrier and cause encepthalopathy leading to dementia.
7. Pediatric AIDS
Viral
transmission may occur to the fetus in
pregnancy. Many of the infected children
may not survive for a year. Children may also acquire the infection from blood
transfusion or blood products.
Laboratory Diagnosis
Lab
diagnosis of HIV infection include tests for immuno deficiency in HIV
infection.
A. Immunological tests
i. Total
leukocyte and lymphocyte count to demonstrate leucopenia and a lymphocyte count
usually below 2000/ mm3.
Ii, Platelet
count will show thrombocytopenia.
iii. Raised
IgG and IgA levels
B. Specific tests for HIV infection
1. Antigen detection
Single
massive infection, as by blood transfusion, the virus antigens may be detectable in blood after about two weeks.
The major core antigen p24 is the virus marker in blood.
2. Polymerase Chain reaction
It is the
most senstitive and specific test.
3. Antibody detection
Demonstration
of antibodies is the simplest and
widely employed technique. It takes 2–8 weeks to months for antibodies to
appear after infection, during this period, the individual may be highly
infectious. This sero negative infective stage is known as the ‘window period’.
Antibody can be detected by.
1. ELISA
2. Western
blot test.
Treatment
The
treatment of AIDS include:
1. The treatment and prophylaxis of infections and
tumours
2. General management
3. Immunorestrorative measures
4.Specific anti-HIV agents
Effective
drugs are available, they are Zidovudine, Didanosine, Zalcitabine, Lamivudine
and Protease inhibitors like Saquinavir, Ritonavir, Indinavir used as
monotherapy or in various combination.
Related Topics