Chapter: Basic Radiology : Gastrointestinal Tract
Gastrointestinal Tract: Normal Imaging
NORMAL IMAGING
Upper Gastrointestinal Tract
The organs that can be examined
in the upper gastrointesti-nal tract include the pharynx, esophagus, stomach,
and duo-denum. The pharynx and esophagus may be evaluated separately or as part
of more complete examinations of these organs. Various techniques are available
to assess the func-tion and structure of the pharynx depending on the
indica-tions for the examination. Motion recording (now using mainly digital
technology) of pharyngeal function and im-aging of pharyngeal structures are
often combined for a more thorough examination. Also, materials of variable
vis-cosity can be used in patients to determine aspiration risk and dietary
needs; the latter is often called a “modifiedbarium swallow” and is done in
conjunction with a swallow-ing therapist. An alternate method of assessing
swallowing is fiberoptic endoscopic evaluation of swallowing (FEES), which is
also performed by a swallowing therapist with training in this technique.
Pharyngeal function is complex
and is best evaluated with motion-recording techniques that allow slow-motion
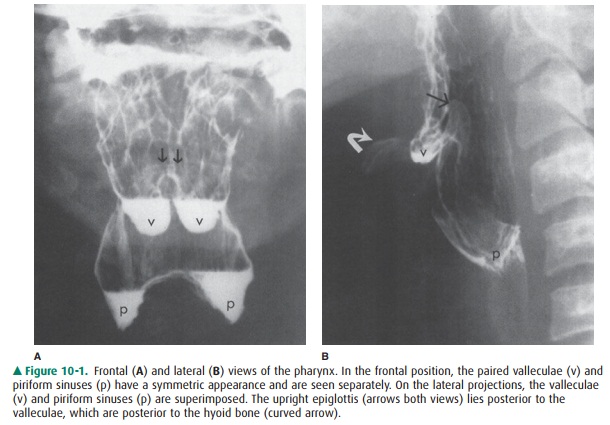
review. Imaging of the pharynx is usually done with the patient in the frontal
and lateral positions (Figure 10-1). In the frontal view, the paired valleculae
and piriform sinuses are sepa-rated. The lateral view of the pharynx
superimposes these structures, but permits better visualization of the base of
the tongue, hyoid bone, and epiglottis anteriorly, and the poste-rior
pharyngeal wall and cervical spine posteriorly.
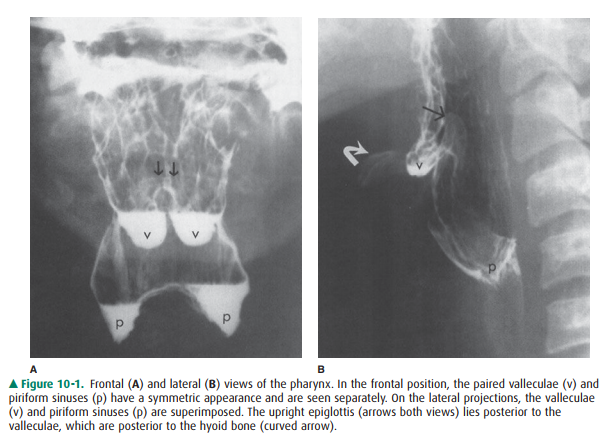
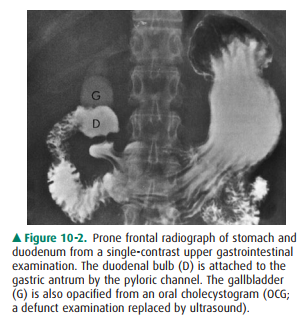
The esophagus, stomach, and
duodenum are usually ex-amined together as part of the upper gastrointestinal
series. A variety of radiographic techniques are used and usually com-bined to
optimize the upper gastrointestinal examination; techniques include observation
of esophageal motility, film-ing of the organs with varying amounts of barium
suspen-sion, gas, or air, and obtaining views of the mucosal surface (Figures
10-2, 10-3). The upper gastrointestinal tract is bestexamined by luminal
contrast studies or endoscopy because mucosal abnormalities are often the cause
of disease. CT and MR imaging can also evaluate these organs and detect focal
masses, wall thickening, and extrinsic processes, such as an invasive
pancreatic malignancy. These modalities can also contribute to the staging of
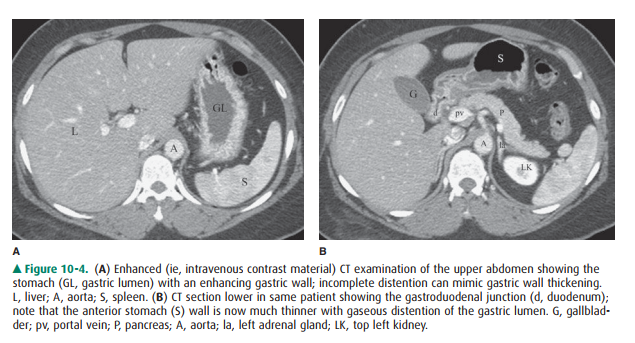
malignancies, especially in the esophagus (Figure 10-4).
The esophagus consists mainly of
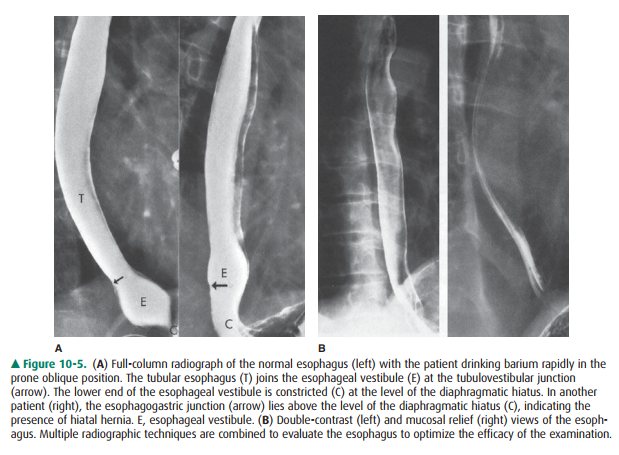
a tubular portion with a bell-shaped termination called the esophageal vestibule. The esophagogastric junction normally lies within or below the esophageal hiatus.
When the esopha-gogastric junction lies above the hiatus, hiatal hernia is
present, which is the most common structural abnormality of the upper
gastrointestinal tract (Figure 10-5 A). The esophageal mucosal surface has a
smooth appearance when distended and shows smooth, thin longitudinal folds when
collapsed (Figure 10-5 B). Esophageal peristalsis can be ob-served by having
the patient swallow single volumes of bar-ium suspension.
The stomach has a complex shape
and varies considerably depending on the degree of distention (see Figures
10-2, 10-3). When the stomach is collapsed, the rugal folds are seen
prominently and may mimic focal or diffuse gastric disor-ders, whether on
luminal contrast or CT studies. With gastric distention, the rugal folds are
flattened and the mucosal sur-face of the stomach is seen more effectively.
Barium studies of the upper gastrointestinal tract evaluate gastric function
poorly; radionuclide gastric emptying studies are more effec-tive for this
purpose.
The duodenum is attached to the
stomach at the narrow pylorus and consists of the duodenal bulb and the
de-scending and ascending portions, although a horizontal segment is often added
(Figure 10-6; see Figure 10-4 B). The duodenum terminates at the duodenojejunal
junction, which is attached to the ligament of Treitz. The duodenal bulb has a
triangular or heart-shaped appearance normally tapering to the apex of the bulb
with its junction to the de-scending portion. The bulbar mucosal surface is
normally smooth. The duodenum assumes a C-shape configuration within the upper
abdomen, and the mucosal folds are sym-metric. The duodenum is surrounded by
many structures, particularly the pancreas, and is often involved secondarily
by diseases in other adjacent organs; cross-sectional CT or MR imaging is
useful in demonstrating this involvement (see Figure 10-4).

Small Intestine
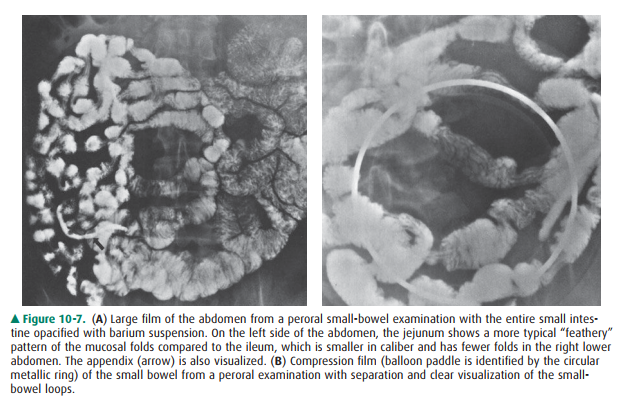
The radiographic examination of
the small bowel evaluates the mesenteric portion of the organ, which consists
of the jejunum and ileum. The following luminal contrast meth-ods can be used
to examine the small intestine: (1) peroral small-bowel series; (2)
enteroclysis; and (3) various retro-grade techniques (eg, via an ileostomy).
The peroral small-bowel series is often done immediately after an upper
gastrointestinal examination and following ingestion of additional barium
suspension. Serial images of the ab-domen are obtained, and abdominal
compression applied to better visualize the small-bowel loops, including the
terminal ileum (Figure 10-7). However, the peroral small-bowel study is
probably the least effective method of exam-ining this organ; techniques that
better distend the small bowel with higher volume are now preferred depending
on the indications. These include enteroclysis and CT or MR imaging with volume
instillation by oral ingestion or via a tube, that is, CT or MR enterography or
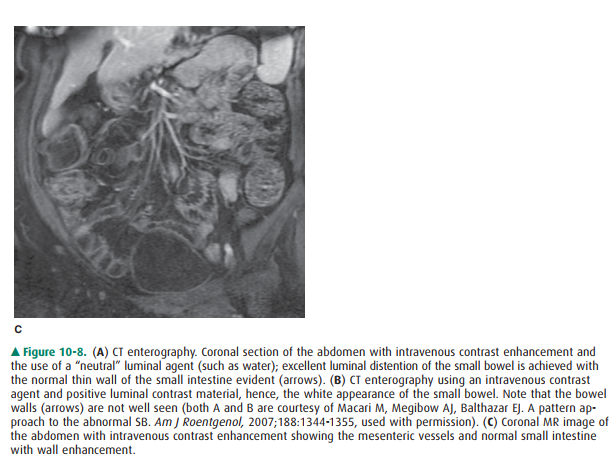
CT or MR entero-clysis (Figure 10-8).
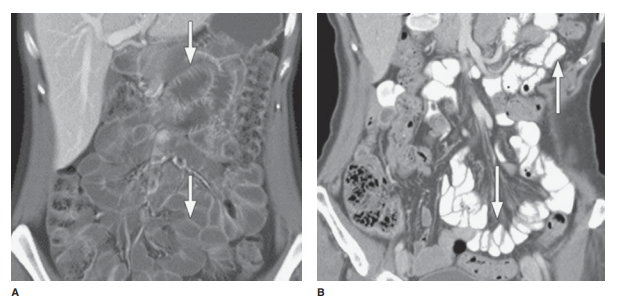
Enteroclysis is an intubated
examination of the small in-testine and can be done by a variety of techniques
and using a number of different modalities (as discussed earlier). The small
intestine is intubated by a nasal or oral route with a small-bore enteric tube
placed with fluoroscopic guidance. A variety of luminal contrast methods exist,
but filming is done similarly to the peroral examination. The enteroclysis
tech-niques permit better control of small-bowel distention and more exact
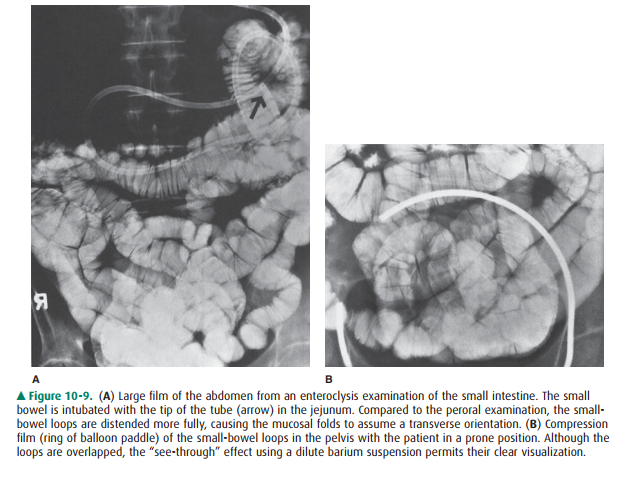
visualization of small-bowel loops (Figure 10-9).
Retrograde examination of the
small bowel involves filling of the organ from the opposite direction. Various
techniques can be used depending on the patient’s anatomy. Reflux of the small
intestine through the ileocecal valve can be done as part of a barium enema. If
the patient has an ileostomy, various devices can be introduced into the ostomy
site and a barium suspension instilled directly.
The length of the mesenteric
small bowel in adults aver-ages about 20 feet, but varies considerably among
individ-uals. The jejunum comprises just over one-third of the length and the
ileum the remainder, although no discrete transition is seen between the two
segments. The normally distended small bowel has a caliber of 2 to 3 cm, being
slightly larger more orad in the jejunum. Depending on the degree of
distention, the mucosal folds (valvulae con-niventes) may have a feathery
appearance or may be trans-versely oriented across the intestinal lumen with
more complete distention. The mucosal folds are more numerous in the jejunum
and gradually decrease in number and size in the ileum.
Large Intestine
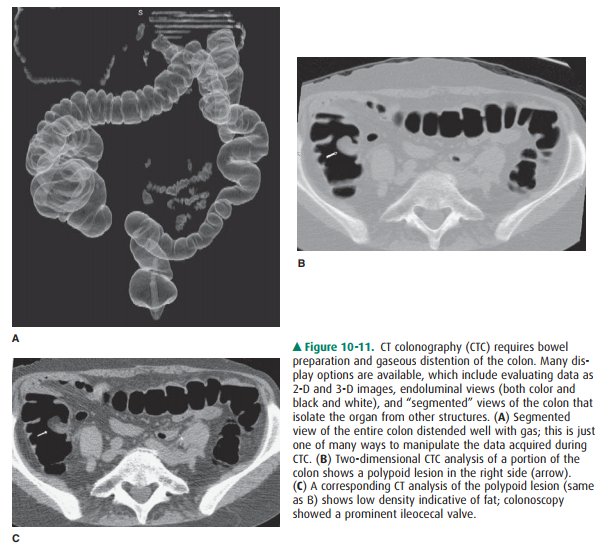
The radiographic examination of
the large bowel evaluates the entire organ from the rectum to the cecum. Reflux
of bar-ium suspension into the ileum and the appendix, if present, occurs
commonly. The colon can be evaluated by several techniques, which include
single-contrast and double-contrast barium enemas; different types of rectal
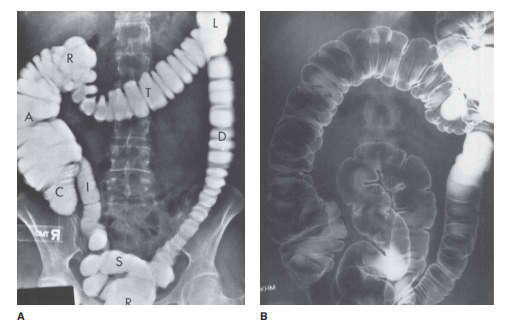
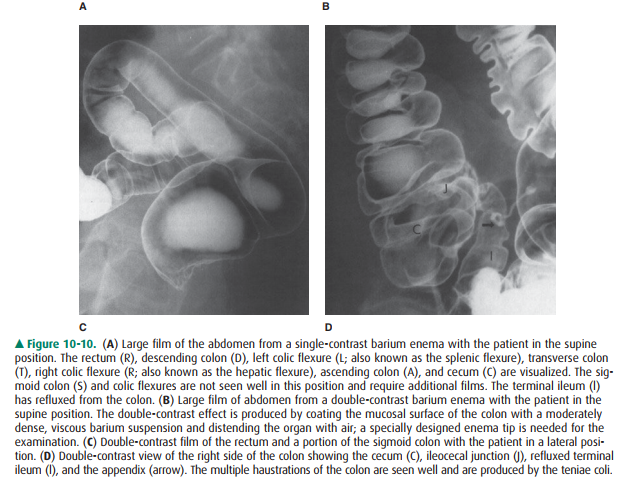
tips and barium suspensions are used for each examination (Figure 10-10). The
single-contrast method simply involves filling the colon with a dilute barium
suspension, whereas the dou-ble-contrast technique requires a denser, more
viscous bar-ium suspension and air. In both methods, large and small
compression images of all segments of the colon are ob-tained. Colonoscopy and
CTC have both had a substantial impact on the numbers of barium enemas now being
per-formed (Figure 10-11).
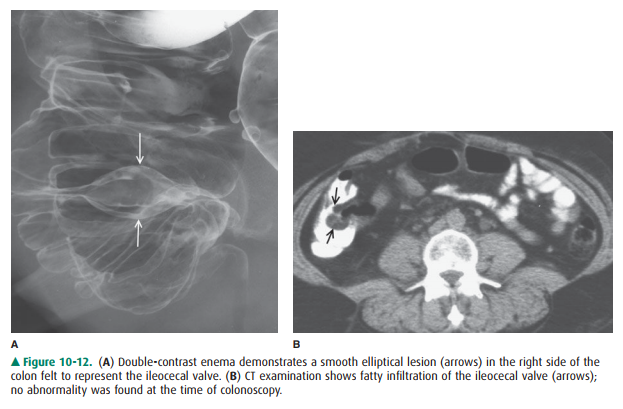
The large intestine consists of
the rectum, sigmoid colon, descending colon, splenic flexure, transverse colon,
hepatic flexure, ascending colon, and cecum (see Figure 10-10). The length of
the colon varies considerably, mainly because of differences in length and
redundancy of the sigmoid colon and colic flexures. The colon also varies in
caliber depending on location and luminal distention achieved. The mucosal
surface has a smooth appearance, and the colonic contour is indented by the
haustra, which are less numerous in the de-scending colon. The rectal valves of
Houston are often seen, especially on double-contrast imaging. The ileocecal
valve has a variety of appearances and may be large if infiltrated by fat
(Figure 10-12).
Related Topics