Chapter: Clinical Anesthesiology: Anesthetic Management: Maternal & Fetal Physiology & Anesthesia
Fetal Physiology
FETAL PHYSIOLOGY
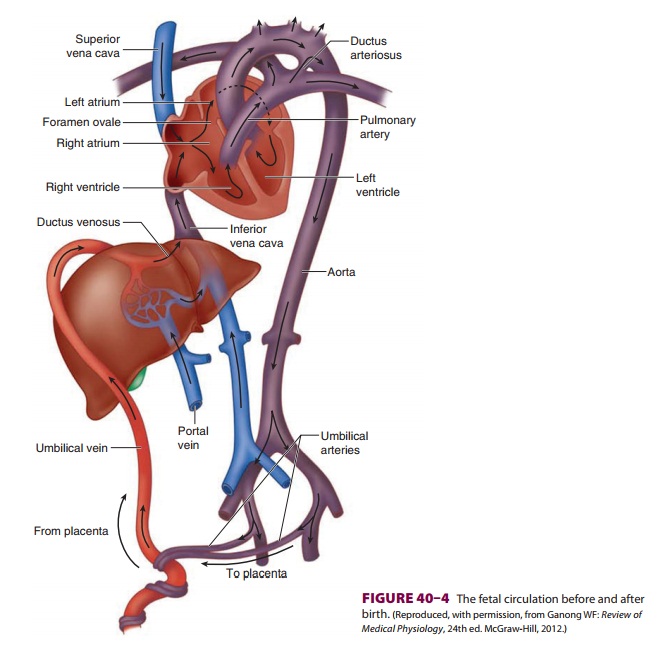
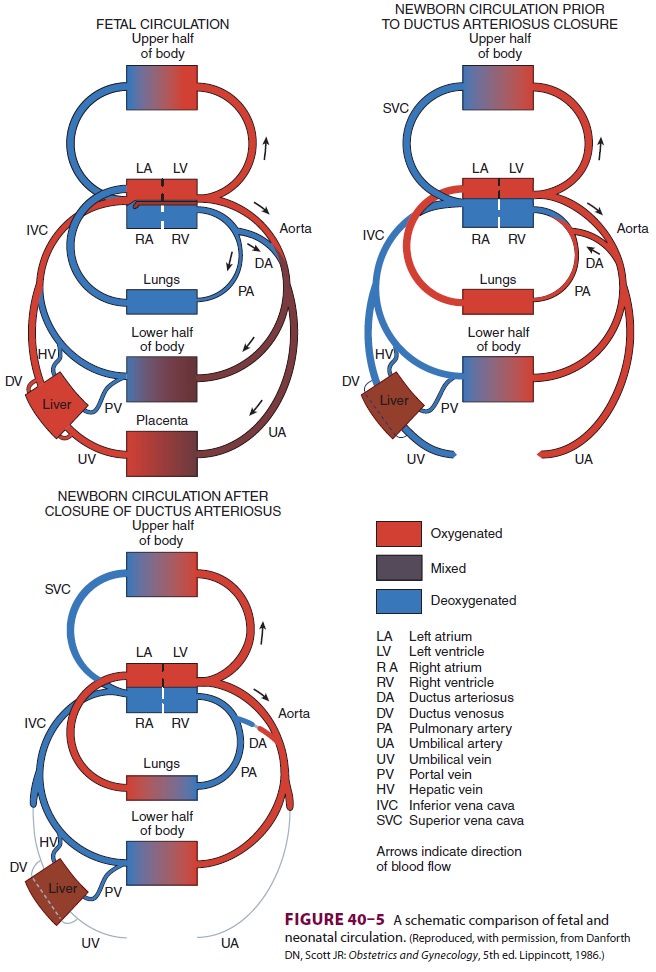
The placenta, which receives nearly half the fetal cardiac output, is
responsible for respiratory gas exchange. As a result, the lungs receive little
blood flow and the pulmonary and systemic circula-tions are parallel instead of
in series, as in the adult (Figures 40–4 and 40–5). This
arrangement is made possible by two cardiac shunts—the foramen ovale and the
ductus arteriosus:
·
Well-oxygenated blood
from the placenta (approximately 80% oxygen saturation) mixes with venous blood
returning from the lower body (25% oxygen saturation) and flows via the
inferior vena cava into the right atrium.
·
Right atrial anatomy
preferentially directs blood flow from the inferior vena cava (67%
oxygen saturation) through the foramen ovale into the left atrium.
·
Left atrial blood is then pumped by
the left ventricle to the upper body (mainly the brain and the heart).
·
Poorly oxygenated blood from the
upper body returns via the superior vena cava to the right atrium.
·
Right atrial anatomy preferentially
directs flow from the superior vena cava into the right ventricle.
·
Right ventricular blood is pumped
into the pulmonary artery.
·
Because of high pulmonary vascular
resistance, 95% of the blood ejected from the right ventricle (60% oxygen
saturation) is shunted across the ductus arteriosus, into the descending aorta,
and back to the placenta and lower body.
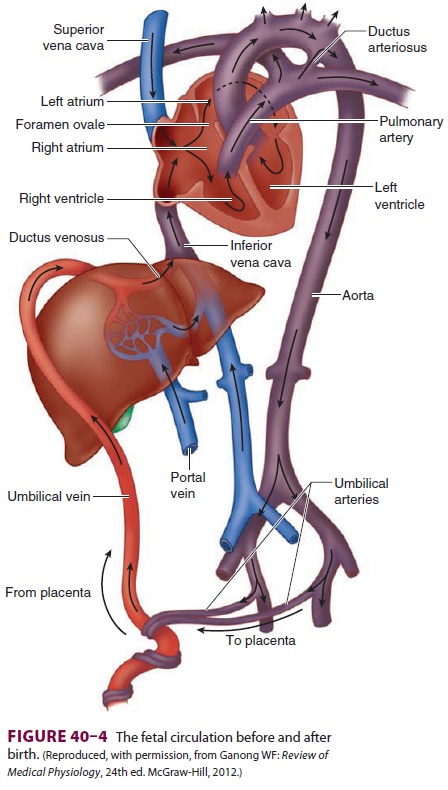
The parallel circulation results in unequal ven-tricular flows; the
right ventricle ejects two thirds of the combined ventricular outputs, whereas
the left ventricle ejects only one third.
Up to 50% of the well-oxygenated blood in the umbilical vein can pass
directly to the heart via the ductus venosus, bypassing the liver. The
remain-der of the blood flow from the placenta mixes with blood from the portal
vein (via the portal sinus) and passes through the liver before reaching the
heart.
The latter may be important in allowing relatively rapid hepatic
degradation of drugs (or toxins) that are absorbed from the maternal
circulation.
In contrast to the fetal circulation, which
is estab-lished very early during intrauterine life, maturation of the lungs
lags behind. Extrauterine survival is not possible until after 24–25 weeks of
gestation, when pulmonary capillaries are formed and come to lie in close
approximation to an immature alveolar epithe-lium. At 30 weeks, the cuboidal
alveolar epithelium
flattens out and begins to produce pulmonary sur-factant. This substance
provides alveolar stability and is necessary to maintain normal lung expan-sion
after birth . Sufficient pulmo-nary surfactant is usually present after 34
weeks of gestation. Administration of glucocorticoids to the mother may
accelerate fetal surfactant production.
Related Topics