Chapter: Basic Radiology : Liver, Biliary Tract, and Pancreas
Exercise: Pancreatic Inflammation
EXERCISE 11-5.
PANCREATIC INFLAMMATION
11-15. What is the most likely diagnosis in Case 11-15 (Figure
11-59)?
A.
Acute edematous pancreatitis
B.
Pancreatic abscess
C.
Pancreatic phlegmon
D.
Hemorrhagic pancreatitis
11-16. What is the most likely diagnosis in Case 11-16 (Figure
11-60)?
A.
Acute edematous pancreatitis
B.
Hemorrhagic pancreatitis
C.
Gastroduodenal artery pseudoaneurysm
D.
Pancreatic abscess
11-17. What is the most likely diagnosis in Case 11-17 (Figure 11-61)?
A.
Acute edematous pancreatitis
B.
Chronic pancreatitis
C.
Pancreatic phlegmon
D.
Hemorrhagic pancreatitis
Radiographic Findings
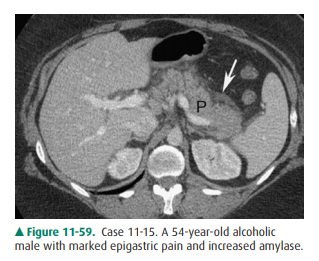
11-15. In this case, the overall size of the pancreas (P) is
en-larged, and the tissue around the pancreas is edema-tous with associated
fluid (arrow). All are findings ofacute edematous pancreatitis (A is the
correct answer to Question 11-15).
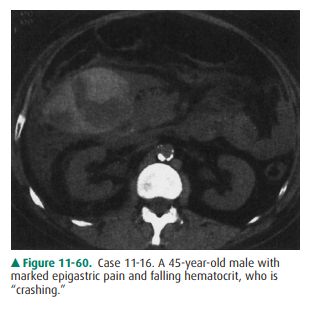
11-16. In this case, peripancreatic inflammatory changes and a
high-density collection are seen adjacent to the pancreatic head, representing
a collection of blood created by hemorrhagic pancreatitis (B is the correct
answer to Question 11-16).
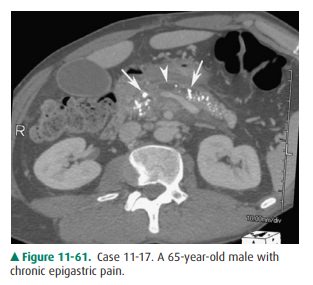
11-17. In this case, multiple calcifications are distributed
throughout the pancreas (arrows) and there is en-largement of the pancreatic
duct (arrowhead) with atrophy of the parenchyma. All are findings of chronic
calcific pancreatitis (B is the correct answer to Question 11-17).
Discussion
Pancreatitis, an inflammatory
condition of the pancreas, has a number of causes including alcohol abuse,
trauma, cholelithiasis, peptic ulcer, hyperlipoproteinemia, hypercal-cemia, and
infection. Pancreatic inflammation may be acute or chronic. Acute pancreatitis
and chronic pancreatitis may not represent different stages of the same
disease.
Acute pancreatitis can occur once
or repetitively and usually has the potential for healing. It can be associated
with mild to severe inflammatory edema (edematous or in-terstitial
pancreatitis) or with hemorrhage (hemorrhagic or necrotizing pancreatitis).
These two forms of acute pan-creatitis may be distinguishable only by the
severity and time course of the disease. Edematous pancreatitis resolves within
2 to 3 days with appropriate therapy, whereas hem-orrhagic pancreatitis
requires much longer to resolve. The diagnosis of simple pancreatitis is
usually based on medical history, physical examination, and laboratory results.
With this information, imaging studies are usually unnecessary, and scans show
the pancreas to be normal or only slightly enlarged. The surrounding fat is
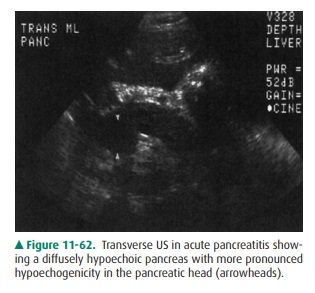
edematous. The pancreas appears hypoechoic on US (Figure 11-62). On CT the
sur-rounding fat appears as areas of streaky interstitial soft-tissue density
in the transverse mesocolon around the pancreas (Figure 11-63).

Clinical criteria to predict the
severity or likelihood of complications of pancreatitis correlate well with the
pres-ence and extent of extrapancreatic abnormalities on imag-ing studies.
Imaging is useful in acute pancreatitis when assessing potential complications.
These complications in-clude hemorrhagic pancreatitis, vascular complications,
phlegmon, and abscess.
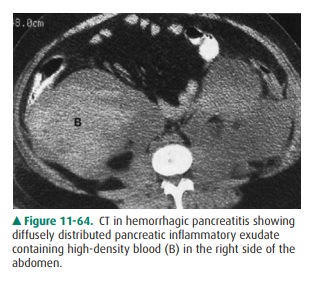
Hemorrhagic pancreatitis is
usually due to erosion of small vessels, is often a serious problem, and
indicates an acutely and critically ill patient. It appears as a collection of
echogenic material on US. On CT, it appears as a collection of high-density
material and can be extremely extensive as it is an aggressive process (Figure
11-64). This material rep-resents the blood.
Large vessels are at risk for
developing pseudoaneurysms when the histiolytic enzymes released by the
inflamed pan-creas erode their walls, leading to a focal, highly vascular
structure within the region of the pancreas. The splenic, gas-troduodenal, and
hepatic arteries are particularly vulnerable. On US and CT, flow within an
enlarged rounded vessel can be seen. Angiography establishes the diagnosis by
showing a focally enlarged vessel, sometimes with extravasation. How-ever, CTA
is also effective for detecting pseudoaneurysms re-lated to pancreatitis.
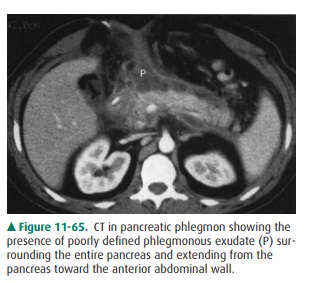
Phlegmon is an inflammatory, boggy, edematous, soft-tissue mass, distinct from fluid, arising from the pancreas and diffusely spreading away from it. Phlegmon appears as diffuse soft-tissue echogenicity or density process sur-rounding the pancreas and contains neither the blood of hemorrhagic pancreatitis nor the fluid of an abscess (Figure 11-65).
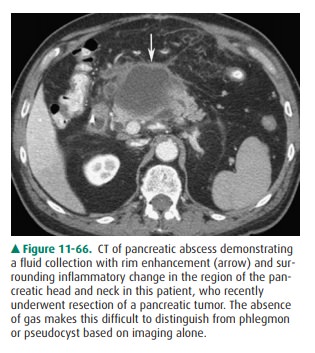
Abscesses are a potentially
life-threatening complication of pancreatitis. Infection associated with
pancreatitis can bethought of as representing infected necrosis (diffuse
infection without pus collection) or pancreatic abscess (collection of pus
surrounded by a capsule). Infected necrosis is harder to identify on imaging
studies than is pancreatic abscess, be-cause it is less distinct and blends
into the surrounding edema. On US, abscess appears as a poorly defined anechoic
or hypoechoic lesion. It enhances sound posteriorly and may contain debris. Gas
appears as a poorly defined echogenicfocus within the nondependent aspect of
the lesion and casts a “dirty” shadow. On CT, the lesion is poorly defined and
may contain gas collections. After contrast material infusion, the border
enhances. If gas is absent, abscess cannot be differen-tiated from phlegmon or
pseudocyst (Figure 11-66). In gen-eral, NM and angiography do not have a major
role in evaluation of acute pancreatitis.
Unlike acute pancreatitis,
chronic pancreatitis is consid-ered to indicate permanent pancreatic damage.
Chronic pancreatitis may or may not be preceded by prior attacks of acute
pancreatitis. The pancreas will develop calcifications within the ductal system
(Figure 11-61). Masslike enlarge-ment of the pancreas can periodically occur,
but often the gland eventually atrophies. The pancreatic duct may dilate. These
findings are visible on both US and CT. NM and an-giography do not have a
current major role in evaluation of chronic pancreatitis.
Related Topics