Chapter: Basic Radiology : Liver, Biliary Tract, and Pancreas
Exercise: Biliary Inflammation
EXERCISE 11-4.
BILIARY INFLAMMATION
11-11. What is the most likely diagnosis in Case 11-11 (Figure
11-45)?

A.
Acute cholecystitis
B.
Uncomplicated cholelithiasis
C.
Chronic cholecystitis
D.
Porcelain gallbladder
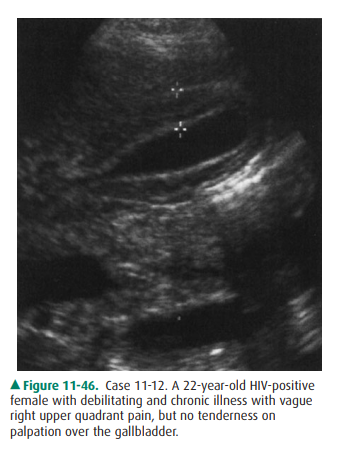
11-12. What is the most likely diagnosis in Case 11-12 (Figure
11-46)?
A.
Oriental cholangiohepatitis
B.
Acquired immunodeficiency syndrome (AIDS)-associated
cholangiopathy
C.
Choledocholithiasis
D.
Porcelain gallbladder
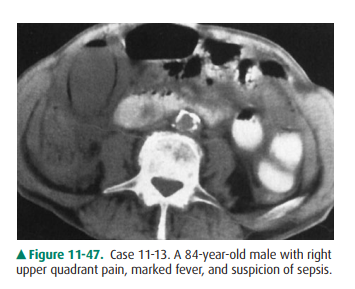
11-13. What is the most likely diagnosis in Case 11-13 (Figure
11-47)?
A.
Acute cholecystitis
B.
Emphysematous cholecystitis
C.
Porcelain gallbladder
D.
Hydrops of gallbladder
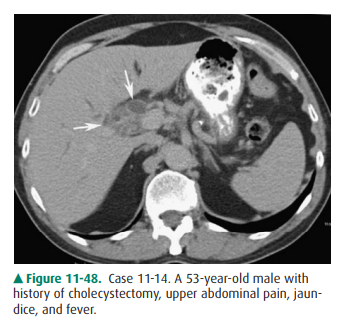
11-14. What is the most likely diagnosis in Case 11-14 (Figure
11-48)?
A.
Choledocholithiasis
B.
Ascending cholangitis
C.
Acute cholecystitis
D.
Emphysematous cholecystitis
Radiographic Findings
11-11. In this case, the gallbladder is distended and the wall
is thickened, measuring more than 5 mm, and has multiple lamina, indicating
gallbladder wall inflam-mation from acute cholecystitis (A is the correct
an-swer to Question 11-11).
11-12. In this case, the gallbladder wall is markedly
thick-ened, measuring over 1 cm, with multiple lamina, but is not tender to
palpation, findings often seen with AIDS cholangiopathy (B is the correct
answer to Question 11-12).
11-13. In this case, gas within the gallbladder wall and lumen
is the primary abnormality, indicating emphy-sematous cholecystitis (B is the
correct answer to Question 11-13).
11-14. In this case, CT demonstrates dilatation of the biliary
ducts with enhancement and thickening of the wall (arrows). In the clinical
setting of fever and jaundice, this most strongly suggests cholangitis (B is
the cor-rect answer to Question 11-14).
Discussion
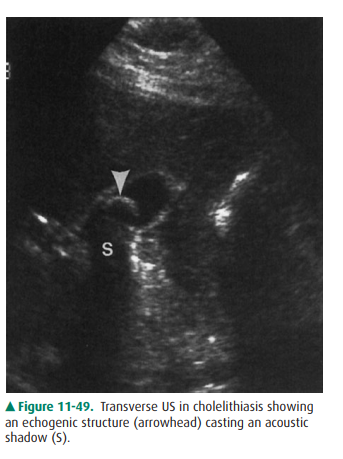
Calculi are a common problem in
the gallbladder and biliary ducts. Cholelithiasis is one of the most common
abdominal disorders overall and is the most common cause of cholecys-titis, as
well as the most common indication for abdominal surgery. Gallstones develop
when the composition of bile, which includes bile salts, lecithin, and cholesterol,
varies from normal and creates supersaturation of cholesterol, which then
precipitates. Historically, patients thought to be harbor-ing gallstones on the
basis of clinical criteria were examined by oral cholecystography, which shows
filling defects in the gallbladder lumen opacified by orally ingested iodinated
con-trast material. However, this examination has been largely re-placed by
sonography, occasionally supported by other imaging information. On US,
gallstones usually appear as mobile, intraluminal, echogenic foci that cast a
well-defined acoustic shadow (Figure 11-49). Two other possible appear-ances
are echogenic foci in the gallbladder fossa without visi-ble surrounding bile
when the gallbladder is contracted, and small, mobile, echogenic foci that do
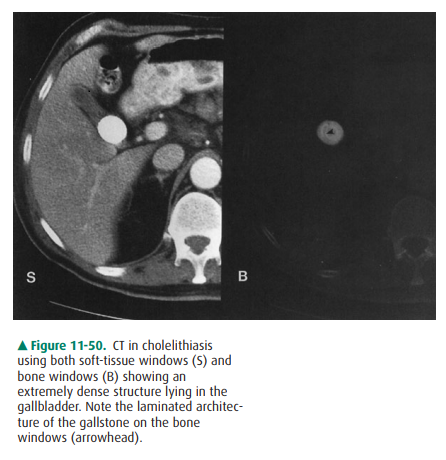
not cast a shadow. On CT, gallstones appear as dense, well-defined,
intraluminal structures (Figure 11-50), but their density can vary from fat
density to near bone density, depending on the relative con-centration of
calcium and cholesterol. Because of their vary-ing density, they can sometimes
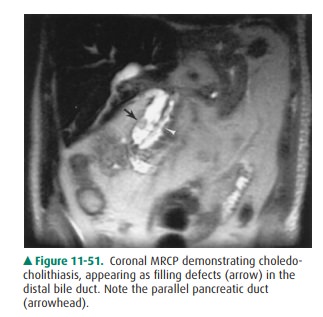
be difficult to see on CT. MR imaging of the biliary system, especially MRCP,
has become more important in biliary imaging, including the detection of
calculi of the gallbladder and biliary tree. Although US re-mains the primary
and initial means of identifying biliary calculi, MRCP can be used as a
supplementary technique, es-pecially in ductal calculi, because imaging of the
biliary treeby US may be suboptimal when obscured by bowel gas. MRCP can depict
the biliary system, filling defects within the biliary tree (Figure 11-51), and
congenital variants of the biliary ducts and is about as accurate as ERCP in
displaying a biliary “road map.” It can also be used to evaluate the biliary
ducts when ERCP is impossible to perform, such as when the patient has
undergone a Billroth procedure, interrupting the continuity of the upper
gastrointestinal tract. NM and angiography have no major role at this time in
assessment of gallstones.
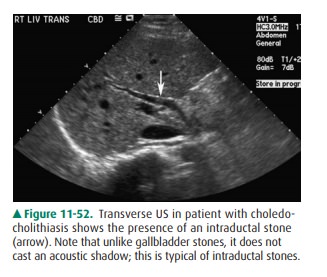
Choledocholithiasis occurs when
calculi pass from the gallbladder into the biliary ducts or when calculi
develop originally within the ductal system. Regardless of origin, they may
obstruct the biliary ducts, cause biliary colic, and lead to cholangitis.
Common duct stones can be evaluated with US, CT, and MRI, or by direct
visualization with ERCP. On US, choledocholithiasis appears as echogenic foci
within the lumen of the biliary duct. Sonographically, common duct stones are
detected less readily than gallbladder stones, and meticulous technique is
required. The entire course of the common bile duct may be technically
difficult or impossible to follow. Choledocholithiasis can cause acoustic
shadows, but for technical reasons these stones are detected less fre-quently
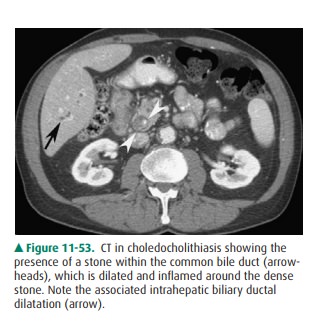
than cholelithiasis (Figure 11-52). On CT, choledo-cholithiasis appears as
intraluminal biliary ductal foci, which, like gallbladder stones, may vary in
density from hypodense to isodense to hyperdense to bile, depending on their
compo-sition (Figure 11-53). On MRCP, choledocholithiasis is seen as a filling
defect in the duct.
Cholecystitis is inflammation of
the gallbladder that is al-most always caused by obstruction of the cystic
duct, usually by an impacted calculus. The inflammation may be acute orchronic,
uncomplicated or complicated, calculous or acalcu-lous. As the gallbladder
continues to accumulate bile, intralu-minal pressure increases and vascular
insufficiency of the wall occurs, causing ischemia, necrosis, and often
superven-ing inflammation. The gallbladder distends, the gallbladder wall
thickens from edema, and the patient is tender to palpa-tion over the
gallbladder (positive Murphy’s sign).
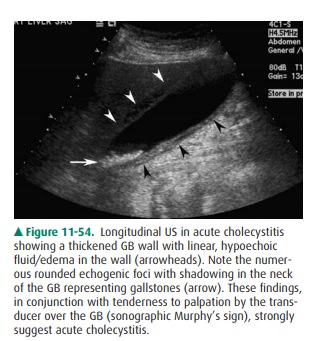
Both ultrasound and hepatobiliary
NM studies are the modalities of choice to evaluate possible cholecystitis.
Sono-graphic signs of acute cholecystitis include cholelithiasis, gallbladder
wall thickening (greater than 3 mm), irregular orlinear hypoechoic structures
within the gallbladder wall, a positive sonographic Murphy’s sign, and marked
gallbladder distention (Figure 11-54). A combination of these signs is a good
positive predictor of acute cholecystitis. In marked chronic cholecystitis, US
shows persistent gallbladder wall thickening or sludge, stones, and contraction
of the gallblad-der. However, in the presence of cholelithiasis, the
gallbladder almost always shows signs of chronic inflammation histolog-ically,
even without symptoms or sonographic findings.
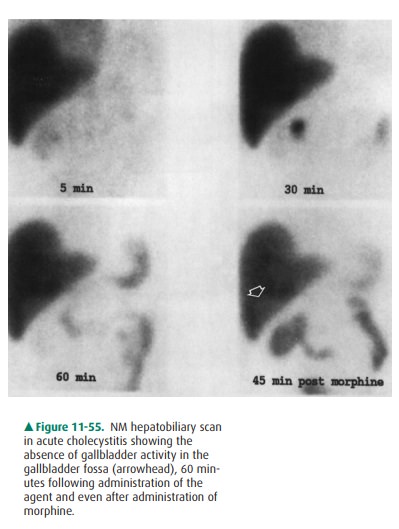
Hepatobiliary NM HIDA scans
depict acute cholecystitis as an absence of filling of the gallbladder with the
radionu-clide once it is excreted by the liver into the biliary ducts; this
absence of filling is due to the obstruction of the cystic duct lumen by
inflammatory edema of the cystic duct wall (Figure 11-55). Sufficient time must
be given to fill the gallbladder. This time interval depends upon whether or
not morphine is administered. Morphine increases the tone of the sphincter of
Oddi and increases intraluminal common bile duct pressure to overcome the
resistance to bile flow into the gallbladder in chronic cholecystitis, but not
in acute cholecystitis when a stone obstructs the duct. Acute cholecystitis is
diagnosed when absence of activity is noted either 45 minutes after morphine
augmentation or after 4 hours without morphineaugmentation. Delayed gallbladder
visualization after 1 hour usually reflects chronic cholecystitis. On CT, the
morphologic findings in patients with acute cholecystitis are similar to the US
findings, including gallstones and thickened and inhomo-geneous gallbladder
wall. However, CT is not as sensitive as US or NM either to the presence of
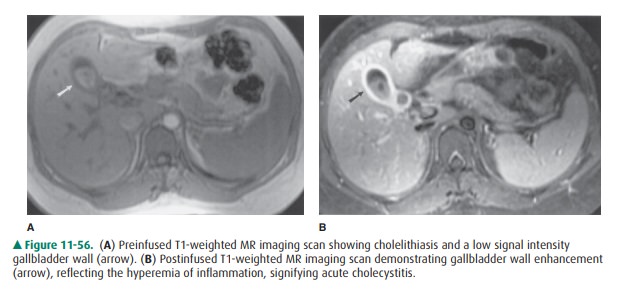
gallstones or to acute cholecystitis. MR imaging can depict the presence of
gallblad-der wall inflammation in the absence of wall thickening by
demonstrating wall enhancement following Gd infusion (Figure 11-56). The exact
role of MR imaging in cholecystitis has not yet been completely evaluated.
Angiography has no role in the diagnosis of cholecystitis.
Many potential complications and
conditions are associated with cholecystitis. These include hydrops, porcelain
gallbladder, milk-of-calcium bile, and emphysematous cholecystitis.
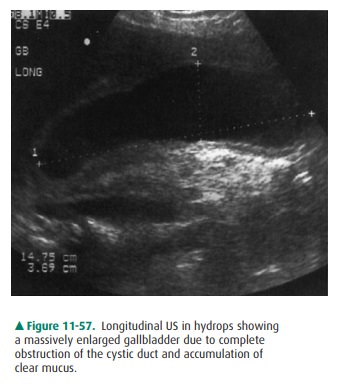
Hydrops refers to the marked
distention of the gallblad-der by clear, sterile mucus, usually under
conditions of chronic, complete cystic duct obstruction. On imaging stud-ies,
the primary finding is enlargement of the gallbladder (Figure 11-57).
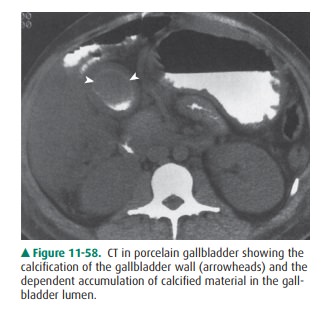
Porcelain gallbladder refers to
calcification of the gall-bladder wall, as a result of chronic inflammation
causing dystrophic calcification and often associated with recur-rent acute
cholecystitis. Gallbladder stones are usually present, and there is a higher
incidence (approximately 10% to 20%) of gallbladder carcinoma. On imaging
stud-ies, complete or incomplete circular wall calcification is present and is
seen as a curvilinear, highly echogenic wall on US or as a curvilinear,
high-attenuation wall on CT (Figure 11-58).
Milk-of-calcium bile refers to a
precipitation of calci-fied material within the lumen of the gallbladder,
usually associated with chronic cholecystitis. US shows echogenic sludgelike
material, possibly with gallstones. CT demon-strates the distinctive appearance
of a horizontal bile-calcium level.
Emphysematous cholecystitis is a
distinctive condition and should be treated as a medical/surgical emergency.
Like acute cholecystitis, it is marked by intense gallbladder wall
in-flammation, but unlike acute cholecystitis, it is not necessar-ily
associated with gallstones. It may be related to ischemia of the gallbladder
wall from small-vessel disease, and it affects an older age group than does
acute cholecystitis. The most common group affected is older diabetic men. Gas
is released by bacterial invasion and accumulates in the gallbladder wall,
lumen, or both. On US, gas is seen as an echogenic focus pro-ducing poorly
defined or “dirty” shadowing behind it. The wall is thickened, perhaps focally,
with gas. On CT, air-density gas is seen within the lumen or wall (Figure
11-47). MR imagingand angiography have no current role in evaluation of these
complications.
Like inflammation of the
gallbladder, inflammation of the biliary ducts, or cholangitis, is an important
clinical con-dition. It is less common than cholecystitis. AIDS-associated
cholangiopathy, ascending cholangitis, and oriental cholan-giohepatitis are three
important forms of cholangitis.
AIDS-associated cholangiopathy is
marked by the fre-quent isolation of opportunistic organisms, including Cryp-tosporidium and cytomegalovirus
from the bile, and by considerable
inflammation of the bile duct wall. On US or CT, the gallbladder or biliary
duct walls may be markedly thickened (greater than 4 mm) (Figure 11-46) and may
contain irregular lamina. Inflammation is present, but stones may or may not be
present. Cholangiography shows irregular stric-tures, papillary stenosis, or
both.
Ascending cholangitis is a
bacterial inflammation of both walls and lumina of the biliary system,
including the gallbladder. It is almost always due to obstruction of the
biliary tract, especially when caused by choledocholithiasis and distal
bile-duct stenosis. The presence of grossly puru-lent material within the duct
indicates suppurative cholan-gitis. Cross-sectional imaging studies are used to
define the level and cause of obstruction. Cholangiography can show the
abnormal biliary ducts directly. The purulent material of suppurative
cholangitis may be seen as echogenic mate-rial on US, high-density material on
CT, or filling defects on cholangiography.
Oriental cholangiohepatitis is a
common illness in en-demic areas of Asia and can be seen in Asian immigrants in
this country. It may be caused by bile duct wall injury from the parasitic
infestation. Ductal stones commonly form, and the ducts are dilated. A
characteristic finding is the presence of intraductal (especially intrahepatic
ductal) cal-culi. These findings are readily demonstrated with US, CT, and
cholangiography.
Related Topics