Chapter: Obstetrics and Gynecology: Cervical Neoplasia and Carcinoma
Evaluation of Abnormal Pap Test Results - Cervical Intraepithelial Neoplasia
Evaluation of Abnormal Pap Test Results
An abnormal cervical cytologic finding from a Pap test should be followed by visual inspection of the vagina and a bimanual examination. The first objective is to exclude the presence of invasive carcinoma. Once this has been accomplished, the objectives are to determine the grade and distribution of the intraepithelial lesion. Options for evaluation include repeat cytology, HPV DNA testing, colposcopy with directed biopsies, and endocervical assessment.
COLPOSCOPY AND ENDOCERVICAL CURETTAGE
Colposcopy
with directed biopsy has been the criterionof disease
detection and remains the technique of choice for treatment decisions. A colposcope is a binocular
stereomi-croscope with variable magnification (usually 7× to 15×) and a light source with a green
filter to aid in the identification of abnormal appearing blood vessels that
may be associated with intraepithelial neoplasia. With colposcopy, areas with
changes consistent with dysplasia are identified, allowing directed biopsy
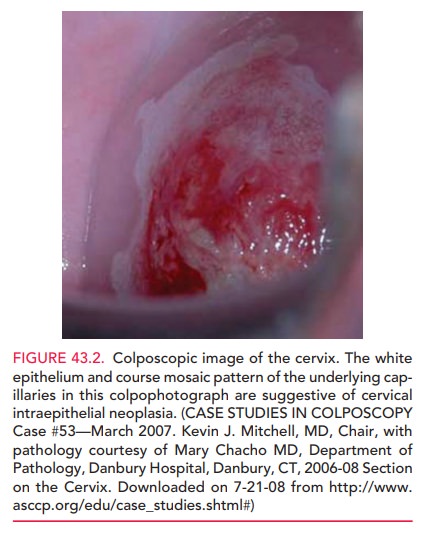
(i.e., biopsy of the area where dysplasia is most likely). Colposcopic criteria
such as white epithelium, abnormal vascular patterns, and punctate lesions help
iden-tify such areas (Fig. 43.2). To facilitate the examination, the cervix is
washed with a 3% to 4% acetic acid solution, which acts as an epithelial
desiccant of intracellular protein, enhancing visualization of dysplastic
lesions. Lesions usu-ally appear with relatively discrete borders near the SCJ
within 10–90 seconds of acetic acid application. Tissue sam-ples for biopsy can
be collected; the number of samples obtained will vary depending on the number
and severity of abnormal areas found.
Visualization of the entire SCJ
is required for a col-poscopy to be considered satisfactory. If the SCJ is not
visualized in its entirety, or if the margins of abnormal areas are not seen in
their entirety, the colposcopic assess-ment is termed unsatisfactory, and other
evaluations such as cervical conization or endocervical
curettage (ECC) is indicated. In this procedure, a small curette is used to
collect cells from the endocervical canal. An endocervical brush can be used to
retrieve additional cells dislodged in the curette specimen. This endocervical
sample is obtained so that potential disease farther inside the cervical canal,
which is not visualized by the colposcope, may be detected. The cervical
biopsies and ECC are then submitted sepa-rately for pathologic assessment.
HUMAN PAPILLOMAVIRUS DNA TESTING
Testing for the presence of high-risk HPV DNA is now being used as an adjunct screening tool for cervical neoplasia in women older than 30 years of age. It is also used as a triage tool for women with Pap test results reported as ASC-US and in the management of non-adolescent women with LSIL.
HPV DNA can identify women whose Pap test results are caused by other,
non-HPV-associated phenom-ena, such as infection, thus preventing unnecessary
colpo-scopic evaluations. Because HPV is more prevalent in younger women and
the rate of CIN 2 and CIN 3 increases with age, HPV DNA testing is more useful
as a triage tool in older women. HPV DNA testing is also used in the ini-tial
workup of women with AGC.
Related Topics