Chapter: Obstetrics and Gynecology: Cervical Neoplasia and Carcinoma
Etiology of Cervical Intraepithelial Neoplasia
CERVICAL INTRAEPITHELIAL NEOPLASIA
Etiology
Cervical cancer and CIN are
caused by human papillo-mavirus (HPV). Of the approximately 80 types of HPV,
about 30 infect the anogenital tract. Approximately 15 of these types (16, 18,
31, 33, 35, 39, 45, 51, 52, 56, 58, 59, 68, 73, and 82) are associated with
cancer and are known as high-risk HPV
types. The majority of cervical cancers are caused by just four of these
high-risk HPV types: 16, 18, 31, and 45. Low-risk HPV types are not associated
with cancer. However, low-risk types 6 and 11 are associ-ated with genital warts (condylomata acuminata) and with low-grade squamous intraepithelial
lesions.
HPV infects the cells of the
cervix. The size and shape of the cervix change depending on age, hormonal
status, and number of children (parity). In reproductive-age women, the cervix
measures 7–8 mm at its widest point. The upper part of the cervix that opens
into the endome-trial cavity is called the internal
os; the lower part that opens into the vagina is called the external os. The exte-rior portion of
the cervical canal is called the exocervix,
and the interior cervical canal is called the endocervical canal. The walls of the endocervical canal contain
numerous folds and plicae.
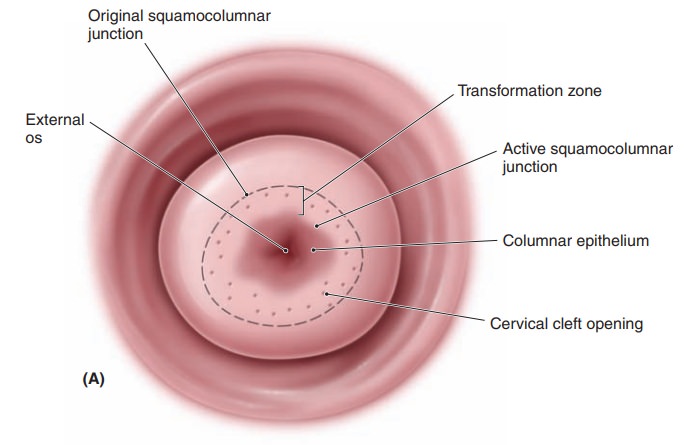
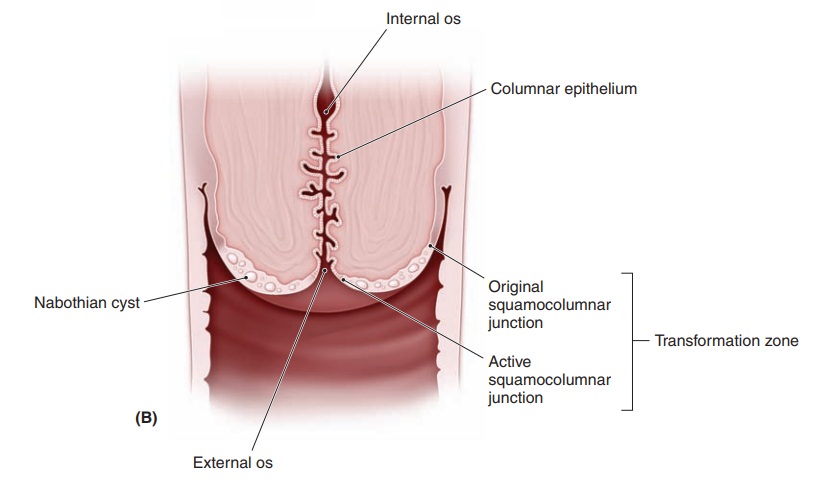
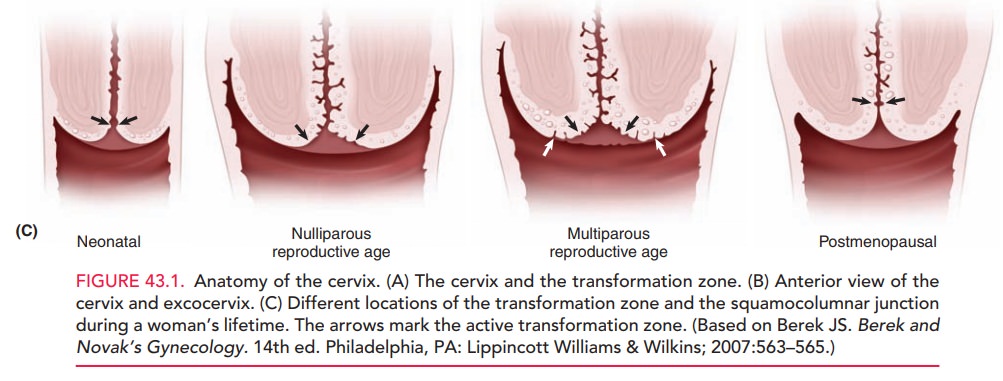
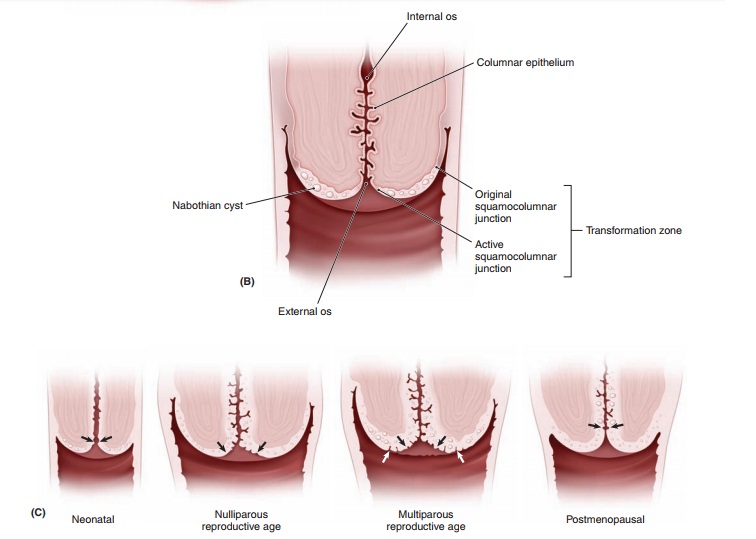
The histology of the cervix is complex (Fig. 43.1, A and B). Overlying the fibrous stroma of the cervix is the cervical epithelium, a meshwork of cells. The epithe-lium is of two types: columnar (glandular) and stratified non-keratinizing squamous epithelia. The columnar epithe-lium consists of a single layer of mucus-secreting cells that are arranged into deep folds or crypts. The area where the two types of epithelia meet is called the squamocolumnarjunction (SCJ). The SCJ is clinically important, as it isthe site where over 90% of lower genital tract neoplasias arise. During childhood, the SCJ is located just inside the external os. Under the influence of hormones and the acidification of the vaginal environment during puberty, subcolumnar cells undergo metaplasia, a process of trans-formation. The metaplasia of these cells causes the SCJ to “roll out,” or evert, from its original position inside the external os to a position on the enlarged cervical surface. Columnar epithelium is also rolled onto the cervical sur-face, where it is exposed to vaginal secretions, irritants, and a changing hormonal milieu. The area between the original SCJ and the active SCJ is called the transforma-tion zone (TZ). As metaplasia continues, the metaplasticepithelium covers and eventually becomes indistinguish-able from the original squamous epithelium.
Glands within the columnar epithelium
may become trapped dur-ing this metaplastic activity by squamous epithelium,
caus-ing Nabothian cysts. These
cysts are not considered pathologic, but a normal consequence of the dynamic
his-tology of the cervix.
The metaplastic cells within the
TZ represent the newest and least mature cells in the cervix, and it is thought
that they are the most vulnerable to oncogenic change. The rate of metaplasia
is highest during adolescence and early pregnancy. During perimenopause, the
new SCJ recedes upward into the endocervical canal, often out of direct visual
contact (Figure 43.1C).
HPV infection of cervical cells
may or may not result in neoplastic change. Most HPV infections are transient,
indicating that the host’s immune system is able to eradi-cate the virus before
it can cause neoplastic changes in cer-vical cells. It is likely that several
as-yet unidentified host or environmental factors act as cofactors. If the HPV
DNA is not integrated into the host genome, encapsulated virions are produced
that are expressed morphologically as “koilocytes.” If HPV DNA is integrated
into the host DNA, the expression of the cell’s regulatory genes may be
altered, leading to the transformation of the cells into intraepithelial lesions
or cancer.
Related Topics