Chapter: Obstetrics and Gynecology: Cervical Neoplasia and Carcinoma
Classification - Cervical Intraepithelial Neoplasia
Classification
The goal of all cervical cancer
classification systems is to establish management guidelines that decrease the
like-lihood of progression of precursor lesions to more advanced lesions. The
2001 Bethesda System is the most widely used system in the United States for
reporting and classifying cervical cytologic studies. Established in 1988 and
updated in 1991 and 2001, The Bethesda Classification outlines the various
possible results of the Pap test, specifies accepted methodologies of reporting
the Pap results, and provides for interpretation of findings. This
categorization allows for defined management options regarding the initial
results of the Pap test (Box 43.2).
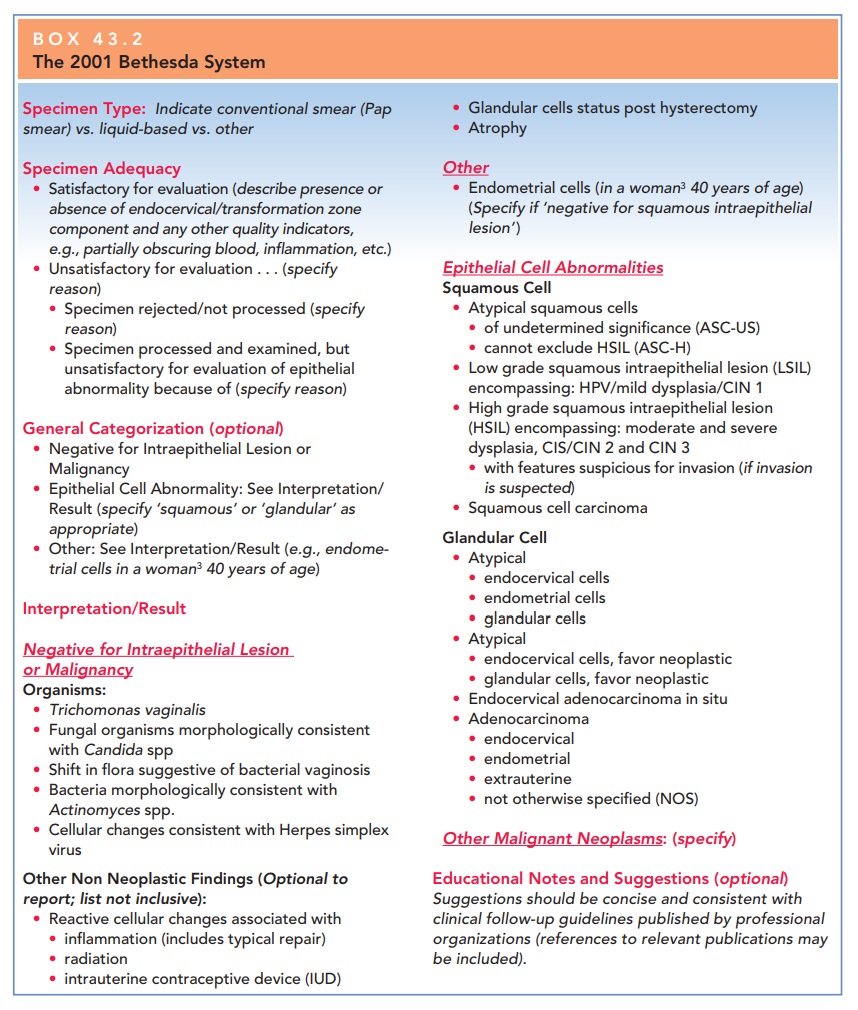
The classification used by the
Bethesda system divides epithelial lesions into two categories: squamous
lesions and glandular lesions. In both categories, lesions are either
precancerous or cancerous. Squamous precursor lesions are described as either atypical squamous cells (ASC),low-grade
squamous intraepithelial lesions (LSIL) or high-grade squamous intraepithelial lesions (HSIL), while
cancerous lesions are termed invasive
squamous car-cinoma. ASC is further divided into ASC of undetermined significance (ASC-US), and ASC–cannot exclude HSIL (ASC-H). Precancerous glandular lesions
are classified as atypical (AGC);
atypical, favor neoplastic; and
endo-cervical adenocarcinoma in situ (AIS). Cancerous glan-dular lesions
are classified as adenocarcinoma.
AGC is also classified as endocervical, endometrial, or not other-wise
specified (NOS).
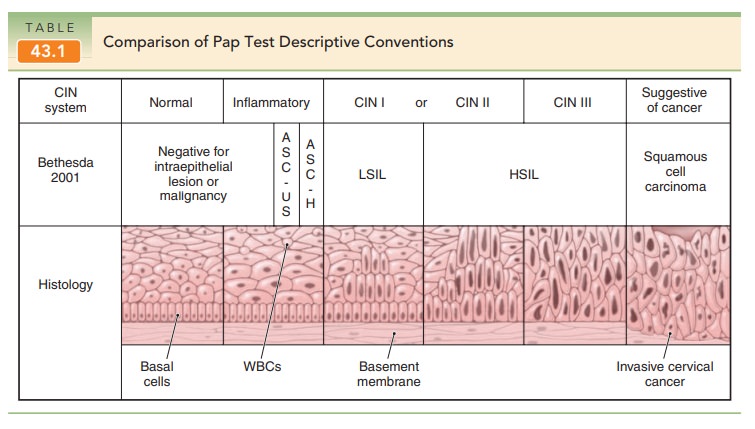
Before the intraepithelial lesion terminology was cre-ated, the term cervical intraepithelial neoplasia (CIN) was used, and lesions were graded as CIN 1, CIN 2, or CIN 3.
The CIN classification system replaced an even earlier classification scheme
that used the term dysplasia and
classified precancerous lesions as mild, moderate, or severe. With each
revision, the terminology for cervical cancer results has become more precise
and reflects the cur-rent scientific understanding of the progression of
cervical cancer. The CIN terminology, however, is still used with the current
Bethesda terminology. LSIL encompasses HPV infection, mild dysplasia, or CIN 1.
HSIL encom-passes CIN 2 and CIN 3. CIN 3 is also designated carci-noma in situ
(Table 43.1).
Despite decades of study, the natural history of cervi-cal intraepithelial lesions is still not completely understood.
The once widely held concept that
low-grade lesions are necessary precursors to the high-grade lesions that, in
turn, may progress to invasive cancer has been questioned as the sole
pathogenesis. It has been observed, for example, that many women present with
CIN 2 or CIN 3 without prior CIN 1 lesions. Although multiple longitudinal
studies have attempted to document rates of “progression” and “regres-sion” of
CIN, results of these studies must be interpreted with caution due to varying
methods of diagnostic criteria, populations, and duration of follow-up.
Related Topics