Chapter: Modern Medical Toxicology: Neurotoxic Poisons: Inebriants
Ethanol: Diagnosis - Inebriant Neurotoxic Poisons
Diagnosis
·
Bedside test—Place 1 ml of unknown solution plus
1ml of acetic acid and 1 drop of H2SO4 in a test tube and
heat gently for 1 minute. A characteristic, strong fruity odour (due to ethyl
acetate) is positive for ethanol.
·
Blood alcohol level—The blood alcohol
concentration(BAC) estimated by immunoassay or gas chromatog-raphy is the
commonest method employed by labora-tories in India. Although accurate, the
results of these tests are often delayed several hours and are not really
appropriate in the clinical scenario.
·
Determine serum electrolytes, glucose, ethanol.
Hypoglycaemia, hypokalaemia, and metabolic acidosis (lactic or ketoacidosis)
may occur.
· BUN, creatinine, liver transaminases, and CPK may be useful in identifying secondary effects, such as hepato-toxicity (chronic ethanol use), respiratory depression, or rhabdomyolysis (if seizures are present).
·
Osmolality: Serum or plasma osmolality allows
estima-tion of blood ethanol level. A blood ethanol concentra-tion of 150 mg%
(32.5 mmol/L) increases osmolality by 21.6 milliosmoles/kg water. The following
equation is said to give good correlation with blood ethanol concentration: BAL
(g/L) = osmolal gap/27
·
Qualitative determination of urinary ethanol is commonly
included in a toxicology screen. However, urinary ethanol levels may be falsely
elevated in patients with diabetes.
Chronic Poisoning (Alcoholism,
Ethanolism):
Alcoholism
is a condition in an individual who consumes large amounts of alcohol over a
long period of time. It is characterised by
––
a pathological desire for alcohol intake –– black-outs during intoxication
–– withdrawal symptoms on ceasing alcohol
intake.
Unfortunately
many patients are not diagnosed correctly as alcoholics by their doctors. A
high index of suspi-cion is important, particularly in cases where there are
repeated consultations for vague symptoms or minor accidents. If in doubt, a
drinking history should be taken in which the patient is asked to describe a
typical week’s drinking.
–– Consumption should be quantified in terms of
units of alcohol. One unit* contains approximately 8 to 10 grams of alcohol and
is the equivalent of half a pint of beer, a single measure (30 ml) of spirits,
or a glass of table wine. Current opinion suggests that drinking becomes a
problem at levels above 21 units/week for men and 14 units/week for women.
Laboratory
tests are useful in confirming alcohol abuse.
Mean
corpuscular volume (MCV) or gamma-glutamyl transpeptidase (gamma GT) is raised
in approximately 50% of problem drinkers.
Medical
complications of alcoholism:
–– GIT—gastritis, periodic diarrhoea,
increased inci-dence of oropharyngeal and oesophageal cancer.
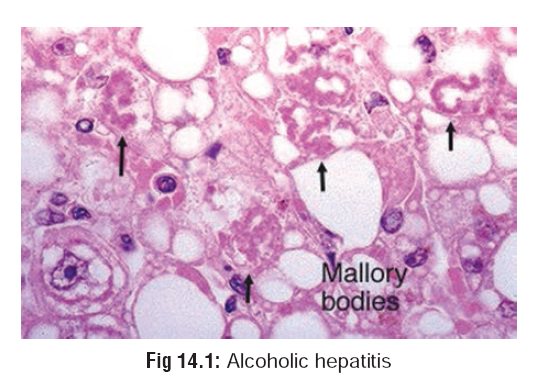
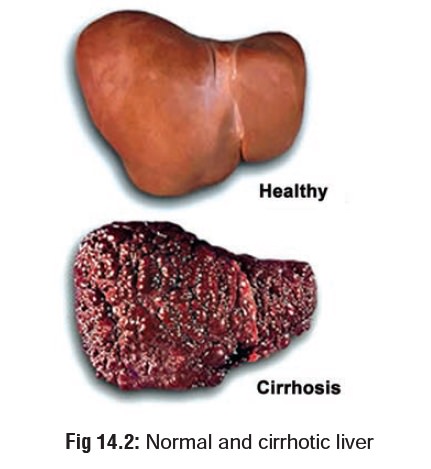
–– Liver—fatty liver with portal hypertension,
hepatitis (Fig 14.1), cirrhosis (Fig 14.2), increased incidence of
hepatic carcinoma.
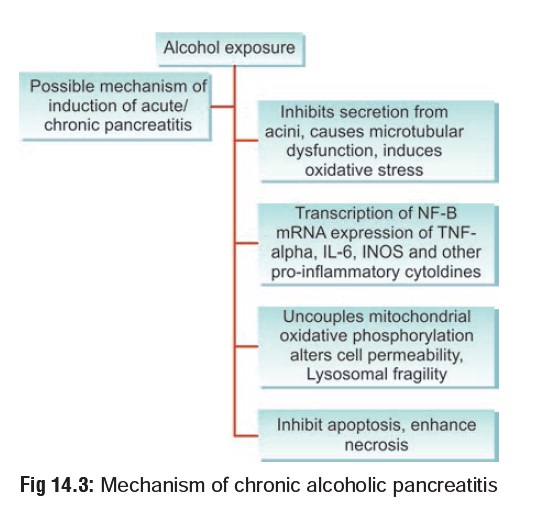
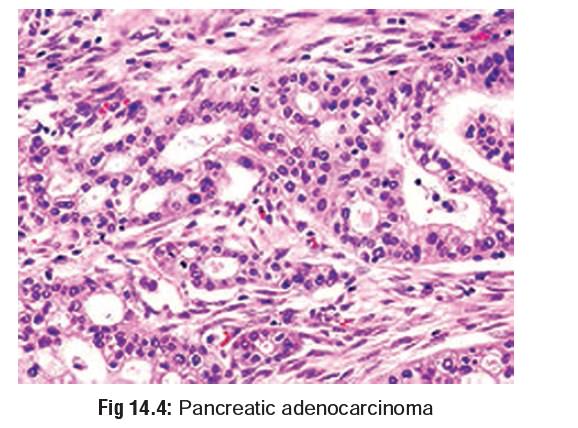
–– Pancreas—acute or chronic pancreatitis
(Fig 14.3), pancreatic cancer (Fig 14.4).
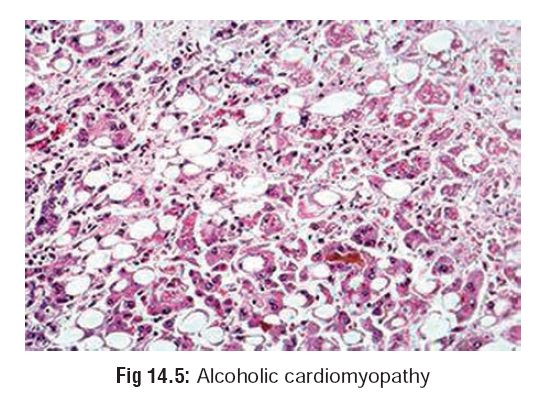
–– CVS—cardiomyopathy (Fig 14.5), dysrhythmias, hypertension.
–– CNS—polyneuropathy, cerebellar
degeneration, demyelination of corpus callosum (Marchiafava-Bignami disease),
amblyopia, stroke.
–– RS—aspiration pneumonia,
alcohol-induced asthma.
–– Endocrine—hypogonadism and
feminisation in males, amenorrhoea, menorrhagia, and infertility in females,
pseudo-Cushing syndrome.
––
Blood—anaemia, thrombocytopenia.
––
Skeletal muscle—myopathy.
–– Neuropsychiatric—memory disturbances
(amnesia, blackout), delusions, delirium tremens, Wernicke’s encephalopathy,
Korsakoff’s psychosis, dementia, alcoholic hallucinosis.
–– Teratogenecity—Foetal Alcohol Syndrome (FAS)— this syndrome is characterised by facial dysmor-phias (Fig 14.6) and other congenital abnormalities, prenatal growth retardation, and neurodevelop-mental abnormalities, including developmental delay or mental retardation, in some children of mothers who abused ethanol during pregnancy.
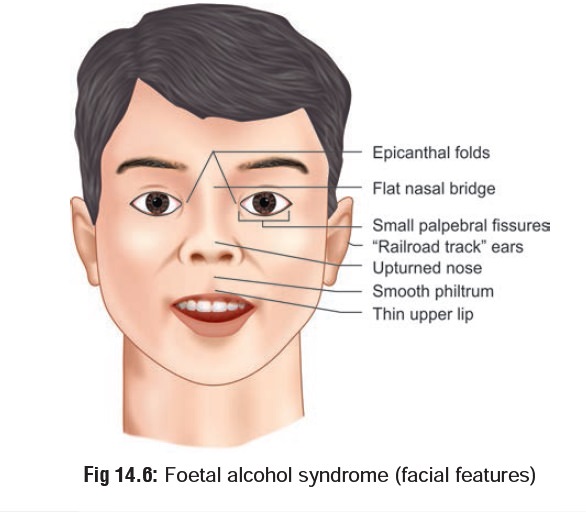
Main abnormalities reported include cleft palate, spina bifida, ventricular and atrial septal defects, tetralogy of Fallot, pulmonary stenosis, and patent ductus arteriosus. Attention deficits, short-term memory, sequential processing deficits, and behavioural problems have been associated with FAS in school-age children.
–– Carcinogenicity—alcohol consumption
has been associated with various cancers, including liver cancer, oesophageal
cancer, breast and prostate cancer, and colorectal cancer.
--Distilled
liquors are more strongly linked with oesophageal cancers than wine or beer.
This may be due to an irritative effect of alcohol on the digestive tract.
--Studies
on the possible relationship between drinking and liver cancer have produced
mixed results: some have shown an association while others have not.
--Ethanol consumption has been
associated with a linear increase in breast cancer incidence in some studies.
--Ethanol has also been implicated
in increasing the risk of cancer of the larynx, oesophagus, mouth, and pharynx
in smokers. Ethanol should be regarded as a possible human co-carcinogen.
--Studies have also indicated a
positive asso-ciation between colorectal cancer and alcohol consumption, mainly
at high levels of alcohol consumption.
Withdrawal syndromes: Sudden
cessation of alcohol intake in a chronic alcoholic can provoke a withdrawal
reaction which may manifest as one of the following: –– Common abstinence
syndrome—
-- Onset : 6 to 8 hours after cessation of
alcohol.
--
Features: Tremor affecting hands, legs, and trunk (“the shakes”),
agitation, sweating, nausea, headache, insomnia.
–– Alcoholic hallucinosis— -- Onset : 24 to 36 hours.
--
Features: Objects appear distorted in shape, shadows seem to move, shouting
or snatches of music may be heard.
--Treatment:
Administration of phenothiazines(e.g. chlorpromazine 100 mg, 8th hourly).
––
Seizures (Rum fits)—
-- Onset : 7 to 48 hours.
--
Features: Clonic-tonic movements, with or without loss of consciousness.
–– Alcoholic ketoacidosis— -- Onset : 24 to 72 hours.
-- Features: Occurs during withdrawal as
well as after episodes of heavy drinking. In many cases there is a preceding
history of GI disturbance such as gastritis or pancreatitis which has led to
sudden diminution of alcohol intake. To compensate for the loss of
carbohydrates and depleted glycogen stores, the body mobilises fat from adipose
tissue as an alternative source of energy. There is a corresponding decrease in
insulin and an increased secretion of glucagon, catecholamines, growth hormone,
and cortisol.
Fatty acids are oxidised and the
final product, acetylcoenzyme A is converted to acetoacetate. This in turn is
converted to beta-hydroxybu-tyrate because of ethanol-induced low redox state.
Volume depletion in these patients inter-feres with the renal elimination of
acetoacetate and beta-hydroxybutyrate and contributes to the acidosis.
Paradoxically, the arterial pH may be normal due to a compensatory respiratory
alkalosis and a primary metabolic alkalosis due to vomiting. Clinical features
include drowsi-ness, confusion, tachycardia, and tachypnoea, progressing to
Kussmaul breathing pattern and coma.
-- Diagnosis:
»» Blood alcohol concentration is
typicallynot high.
»»
Blood glucose may be slightly elevated.
»» Since the nitroprusside reaction
detectsonly acetone and acetoacetate and not beta-hydroxybutyrate, the assay
for ketones is likely to be only weakly positive.
»» There is an elevated anion-gap
metabolicacidosis. Serum ketones are markedly elevated.
»» Hypokalaemia and hypochloraemia
areoften present.
-- Treatment:
»»
Correction of volume depletion—infusionof solutions of normal saline
with dextrose.
»»
Potassium supplementation may be required. »»
Thiamine (50 to 100 mg) to prevent devel-opment of Wernicke-Korsakoff
syndrome.
––
Delirium tremens (DTs)— -- Onset : 3 to 5 days.
-- Features: There is a dramatic onset of
disor-dered mental activity characterised by clouding of consciousness,
disorientation, and loss of recent memory. There are vivid hallucinations which
are usually visual, but sometimes audi-tory in nature. There is severe
agitation with restlessness and shouting, tremor, and truncal ataxia. Insomnia
is prolonged. Autonomic disturbances include sweating, fever, tachy-cardia,
hypertension, and dilated pupils. Dehydration and electrolyte disturbances are
characteristic. Blood testing shows leucocytosis and impaired liver function.
--Treatment:
»»Well lit, reassuring environment.
»»For agitation—diazepam 10 mg IV
initially, and then 5 mg every 5 minutes until full control, followed by 5 to
10 mg orally 3 times daily.
»»Thiamine in the usual dose.
»»Correction of fluid and electrolyte
imbal-ance.
–– Wernicke-Korsakoff syndrome –
This is very rare as a withdrawal phenomenon, and is actually the result of
thiamine deficiency due to impoverished diet in an alcoholic.
--
Features: Wernicke’s encephalopathy is the acute form and is characterised
by drowsi-ness, disorientation, amnesia, ataxia, periph-eral neuropathy,
horizontal nystagmus, and external ocular palsies. It results from damage to
mammillary bodies, dorsomedial nuclei of thalamus, and adjacent areas of grey
matter. When recovery from Wernicke’s encephalop-athy is incomplete, a chronic
amnesic syndrome develops called Korsakoff’s psychosis which is characterised by
impairment of memory and confabulation (falsification of memory).
-- Treatment:
»» For Wernicke’s encephalopathy—
adminis-tration of thiamine 50 to 100 mg IV daily, infused slowly in 500 ml of
fluid for 5 to 7 days, and fluid replacement.
Treatment
Acute Poisoning (Intoxication,
Inebriation):
·
Airway protection, ventilatory
support.
·
Activated charcoal is NOT useful.
·
Stomach wash.
·
Thiamine 100 mg IV
·
Dextrose
–– Indications—If rapidly determined
bedside glucose level is less than 60 mg/100ml, or if rapid determi-nation is
not available.
–– Adult—25 grams (50 ml of 50% dextrose
solution) intravenously; may repeat as needed.
–– Paediatric—0.5 to 1 gram dextrose per
kg as 25% dextrose solution or 10% dextrose solution (2 to 4 ml/kg).
––
Precautions—Glucose administration should necessarily be preceded by
100 mg of thiamine IV or IM if chronic alcoholism or malnutrition is suspected,
to prevent development of Wernicke’s encephalopathy.![]()
·
Intravenous fluids.
·
A variety of drugs have been tried to hasten the elimi-nation
of ethanol or reverse its intoxicating effects, including naloxone,
physostigmine, and caffeine. None of them have been proved to be truly
effective. Recently, flumazenil (3 mg IV) has been shown to be effective (in
experimental studies) in reversing the respiratory depres-sion associated with
ethanol ingestion.
·
Haemodialysis can eliminate ethanol 3 to 4 times more
rapidly than liver metabolism. May be useful in patients with excessive blood
levels, impaired hepatic function and in those whose condition deteriorates in
spite of maximal supportive measures. However, it is unusual for dialysis to be
necessary to treat even severe ethanol intoxication.
Chronic Poisoning:
Treatment of withdrawal—apart from
the treatment measures outlined earlier (vide
supra), the following drugs have also been tried with varying degrees of
success:
–– Carbamazepine—It has been shown
to be effective in treating alcohol withdrawal, including delirium tremens.
–– Chlormethiazole—It is one of the
most popular drugs used for alcohol withdrawal abroad, and is administered in a
rapidly reducing dosage over 6 to 7 days. However it is itself associated with
a strong abuse potential.
–– Clonidine and
gamma-hydroxybutyric acid have also shown promising results in the treatment of
withdrawal symptoms. The former is given at a dose of 60 to 180 mcg/hr IV, and
the latter 50 mg/ kg, orally.
–– One of the most recent entrants
is tiapride, an atyp-ical neuroleptic agent which is a selective dopamine
D2-receptor antagonist. But it should be given only as an adjunct while
seizures, hallucinosis, etc., are being taken care of by other drugs. It is
effective in ameliorating psychologic distress associated with alcohol
abstinence. For delirium, the recommended dose is 400 to 1200 mg/day 6th
hourly, while the maintenance dose subsequently to help abstain from alcohol
should not exceed 300 mg/day.
Aversion therapy—The main aim in the
treatment of alcoholism is to gradually wean away the patient from the clutches
of ethanol, once the acute manifestations of withdrawal have been taken care
of. This process referred to quite loosely as de-addiction or detoxifi-cation,
should be undertaken only after admission to a hospital over a period of
several days, under close medical supervision. The insatiable craving for
alcohol that is often present must be tackled effectively, and![]() usually requires strongly deterrent measures. Many methods
have been tried in this connection, and one of the more succesful ways is to
administer a drug called disulfiram. It is a disulfide molecule
(tetraethylthiuram) which interferes with the oxidative metabolism of ethanol
at the acetaldehyde stage, as a result of which acetaldehyde accumulates
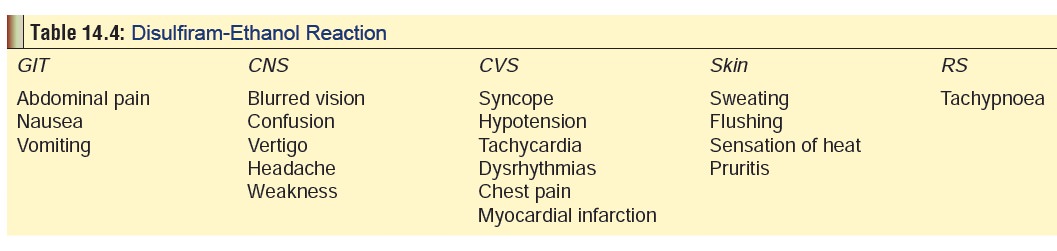
producing unpleasant symp-toms* (Table
14.4).
usually requires strongly deterrent measures. Many methods
have been tried in this connection, and one of the more succesful ways is to
administer a drug called disulfiram. It is a disulfide molecule
(tetraethylthiuram) which interferes with the oxidative metabolism of ethanol
at the acetaldehyde stage, as a result of which acetaldehyde accumulates
producing unpleasant symp-toms* (Table
14.4).
––Principles
of disulfiram therapy—
-- Ensure that the patient is off
alcohol for a minimum period of 12 hours before starting therapy.
-- Administer disulfiram only by the
oral route. -- Warn the patient explicitly that while he is on disulfiram,
alcohol must not be consumed even in small quantity since it can provoke a
severe (and sometimes fatal) reaction. He must also avoid taking medicinal
preparations containing alcohol, including topical preparations.
--The usual dose of disulfiram is
250 mg/day which may have to be taken for an indefinite period of time. Such
chronic use unfortunately often produces side effects like halitosis (rotten
egg odour due to sulfide metabolites), pruritis, headache, drowsiness,
impotence, peripheral neuropathies, depression, mania, psychosis, and
hepatotoxicity. The patient must be closely monitored and dosage reduced if
necessary.
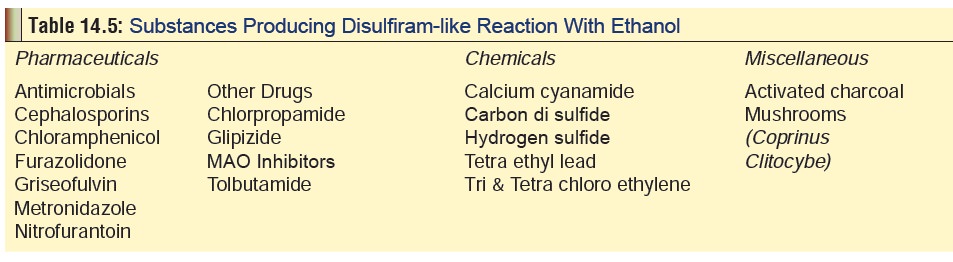
--Other than disulfiram, there are
numerous other substances which evoke a similar reaction with ethanol (Table 14.5).
Supportive psychotherapy—More than
individualised psychotherapy, it is group therapy which is effective in the
long, term management of abstinence. Groups provide an opportunity for
resocialisation and a sense of mutual commitment. Self-support organisations
such as Alcoholics Anonymous (AA)
play an important role. The AA which had its origins in the USA in 1935 now has
more than 53,000 groups spread worldwide including India. The only requirement
for membership is a “desire to stop drinking”. There is no membership fee and
the organisation functions on a self-supporting basis through contributions
from the members. Local addresses of AA groups functioning in a given region
can be located in the telephone directory of that area. Meetings are generally
held once a week and are informal affairs conducted in a friendly atmosphere.
Generally two or three speakers share their experi-ences during each session
relating to their addiction and recovery.
Related Topics