Chapter: Essentials of Psychiatry: Clinical Evaluation and Treatment Planning: A Multimodal Approach
Differential Diagnosis - Clinical Evaluation and Treatment Planning: A Multimodal Approach
Differential Diagnosis
The differential diagnosis is best approached by
organizing the information obtained in the psychiatric evaluation into five
domains of mental functioning according to the disturbances revealed by the
evaluation. After organizing the in-formation into these five domains, the
psychiatrist looks for the psychopathological syndromes and potential diagnoses
that best account for the disturbances described. A complete diagnostic
evaluation includes assessments on each of the five axes of DSM-IV-TR (Table
19.22).
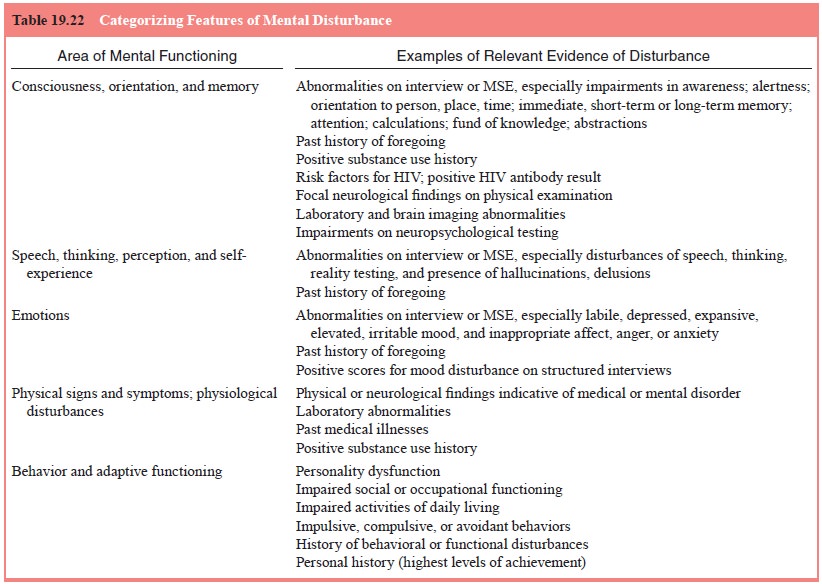
Disturbances of consciousness, orientation and
memory are most typically associated with delirium related to a general medical
condition or a substance use disorder. Memory impair-ment and other cognitive
disturbances are the hallmarks of de- etiology. It is important to elicit risk
factors for HIV infection and, when they are present, to encourage voluntary
HIV anti-body testing. Neuropsychological testing is particularly useful in the
diagnosis of subcortical dementia, such as that caused by Huntington’s disease
and HIV infection. Dissociative disorders and severe psychotic states may also
present with disturbances in this domain without evidence of any medical
etiology. Cognitive impairment caused by mental retardation is established by
intel-ligence testing.
Disturbances of speech, thinking, perception and
self-experience are common in psychotic states that can be seen in patients
with such diagnoses as schizophrenia and mania, as well as in central nervous
system dysfunction caused by substance use or a medical condition. Disturbances
in self-experience are also common in dissociative disorders and certain
anxiety, somato-form and eating disorders. Cluster A personality disorders may
be associated with milder forms of disturbances in this domain (American
Psychiatric Association, 2000).
Disturbances of emotion are most typical of affective
and anxiety disorders. These disturbances may also be caused by substance use
disorders and general medical conditions. Mood and affect disturbances
accompany many personality disorders and may be especially pronounced in
borderline personality disorder.
Physical signs and symptoms and any associated abnor-malities revealed by diagnostic medical tests and past medical history are used to establish the presence of general medical con-ditions, which are coded on Axis III. When a medical disorder is causally related to a psychiatric disorder, a statement of this re-lationship should appear on Axis I. Physical signs and symptoms may also suggest diagnoses of mood or anxiety disorders or states of substance intoxication or withdrawal. Physical symptoms for which no medical etiology can be demonstrated after thorough assessment suggest somatoform or factitious disorders or malin-gering, although the possibility of an as-yet-undiagnosed medical condition should still be kept in mind.
Information about behavior and adaptive functioning
is useful for diagnosing personality disorders, documenting psychosocial and
environmental problems on Axis IV, and as-sessing global functioning on Axis V.
This information is also useful for diagnosing most psychiatric disorders,
which typically include criteria related to abnormal behaviors and functional
impairment.
When all information has been gathered and
organized, it may be possible to reach definitive diagnoses, but sometimes this
must await further evaluation and the development of the comprehensive
treatment plan.
Initial Treatment Plan
The initial treatment plan follows the case
formulation, which has already established the nature of the current problem
and a tenta-tive diagnosis. The plan distinguishes between what must be
ac-complished now and what is postponed for the future. Treatment planning
works best when it follows the biopsychosocial model.
Biological Intervention
This includes an immediate response to any
life-threatening medical conditions and a plan for the treatment of other less
acute physical disorders, including those that may contribute to an al-tered
mental status. Prescription of psychotropic medications in accordance with the
tentative diagnosis is the most common bio-logical intervention.
Psychosocial Intervention
This includes immediate plans to prevent violent or
suicidal be-havior and address adverse external circumstances. An overall
strategy must be developed that is both realistic and responsive to the
patient’s situation. Developing this strategy requires an awareness of the
social support systems available to the patient; the financial resources of the
patient; the availability of services in the area; the need to contact other
agencies, such as child wel-fare or the police; and the need to ensure child
care for dependent children.
Initial Disposition
The primary task of the initial disposition is to
select the most ap-propriate level of care after completion of the psychiatric
evalua-tion. Disposition is primarily focused on immediate goals. After
referral, the patient and the treatment team develop longer term goals.
Hospitalization
The first decision in any disposition plan is
whether hospitaliza-tion is required to ensure safety. There are times when a
patient presents with such severe risk of harm to self or others that
hos-pitalization seems essential. In other cases, the patient could be managed
outside the hospital, depending on the availability of other supports. This
might include a family who can stay with the patient or a crisis team in the
community able to treat the patient at home. The more comprehensive the system
of services, the easier it is to avoid hospitalization. Because hospitalization
is associated with extreme disruption of usual life activities and in and of
itself can have many adverse consequences, plans to avoid hospitalization are
usually appropriate as long as they do not compromise safety.
Day Programs, Crisis Residences and Supervised Housing
These interventions provide ongoing supervision but
at a lower level than that available within the hospital. They are most often
used to treat patients with alcohol and substance use disorders or severe
mental illness. Crisis housing can be useful when a patient cannot safely
return home, when caregivers need respite, and when the patient is homeless.
Other forms of supervised hous-ing usually have a waiting period and may not be
immediately available.
There are many different types of and names for
day-long programming, including partial hospitalization, day treatment,
psychiatric rehabilitation and psychosocial clubs. Depending on the nature of
the program, it may provide stabilization, daily medication, training in social
and vocational skills, and treatment of alcohol and substance use problems.
Long-term day programs should generally be avoided if a patient is functioning
successfully in a daytime role, such as in a job or as a homemaker. In these
instances, referral to a day program may promote a lower level of functioning
than the patient is capable of.
Outpatient Medication and Psychotherapy
The most common referral after psychiatric
evaluation is to psy-chotherapy and/or medication management. In office-based
set-tings, the psychiatrist decides whether she or he has the time and expertise
to treat the patient and makes referrals to other practi-tioners as
appropriate. Hospital staff usually have a broad over-view of community
resources and refer accordingly. There are high rates of dropout when patients
are sent from one setting to another. These can be reduced by providing
introductions to the treatment setting and/or conducting follow-up to ensure
that the referral has been successful.
Comprehensive Treatment Planning
The psychiatric evaluation usually continues beyond
the ini-tial disposition. The providers assuming responsibility for the
patient, who may be inpatient staff, outpatient staff, or private
practitioners, complete the evaluation and take responsibility for developing
the comprehensive treatment plan. This plan covers the entire array of concerns
that affect the course of the patient’s psychiatric problems. In hospital
settings, the initial treatment plan is usually completed within 24 to 72 hours
after admission, followed by comprehensive treatment plan after more extensive
evaluation.
The comprehensive treatment plan usually includes
more definitive diagnoses and a well-formulated management plan with central
goals and objectives. For severely ill or hospitalized patients, every area is
usually covered (Table 19.23 and 19.24). It is best for the patient and, as
appropriate, the family, to have input into the plan. The comprehensive
treatment plan guides and coor-dinates the direction of all treatment for an
extended time, usually
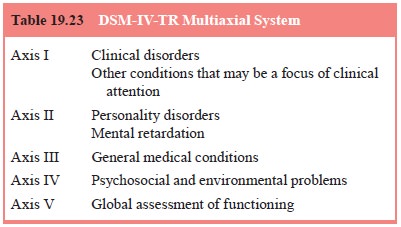
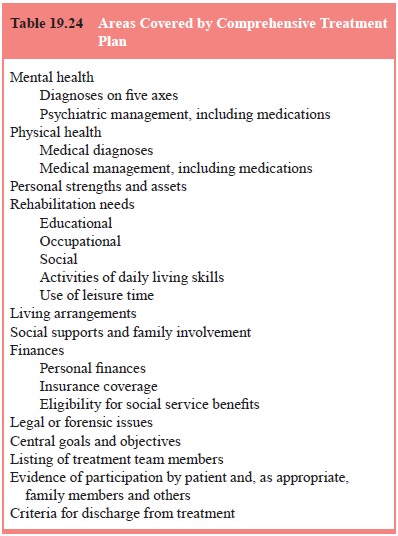
months, and is periodically reviewed and updated.
For more focal psychiatric problems (e.g., phobias, sexual dysfunctions) and
more limited interventions (e.g., brief interpersonal, cognitive, and
be-havioral therapies in office-based practices), the comprehensive treatment
plan may focus on only several of the possible areas.
Related Topics