Chapter: Essentials of Psychiatry: Clinical Evaluation and Treatment Planning: A Multimodal Approach
Limitations of Reliability and Validity
Limitations of Reliability and
Validity
Despite the obvious role of quantification in
neuropsychologi-cal testing, interpretation of test data ultimately depends on
the knowledge base, training and skill of the clinician. Neuropsy-chological
test scores are an indirect measure of the status of the brain, as contrasted
with direct measures of structure by magnetic resonance imaging (MRI) or
function by positron emission tomography (PET), functional MRI, or EEG. In a
psy-chiatric setting, where problems of motivation, effort, coopera-tion and
stage of the illness are ubiquitous, analysis of neuropsy-chological data must
go beyond the level of performance deficits because many studies have shown
performance to be especially affected by functional (emotional) factors.
Process analyses ori-ented to focal syndromes and focused on the relative
efficiency of the two sides of the body and hemispace may enhance predic-tive
validity.
The patient’s clinical state may change, and
repeated test-ing when the patient’s clinical status is optimal often clarifies
the nature of the diagnosis. Selective deficits found in the con-text of
otherwise good performance when patients are tested in their best state can be
considered most valid. Neuropsychologists must also take into account the
effect of medication on neuropsy-chological function and distinguish medication
effects from the patient’s adaptive ability. Different medications are likely
to produce different effects. For example, Trimble and Thompson (1986) have
demonstrated that, for epileptic patients and normal subjects, anticonvulsants
have negative effects on most measures of neuropsychological testing. On the
other hand, Cassens and colleagues (1990) have demonstrated that (traditional)
antipsy-chotic medications have negligible or mildly positive effects on most
measures of neuropsychological testing in chronic schizo-phrenia, with the
exception of a negative effect on motor per-formance. Spohn and Strauss (1989)
have indicated that typical antipsychotic medications tend to improve
attentional perform-ance, such as on versions of the CPT.
Structured Clinical Instruments and Rating Scales
Structured instruments and rating scales have been
developed primarily for research purposes. They allow investigators to compare
findings in different studies by ensuring that similar data and criteria have
been used to establish diagnoses and to measure the presence and severity of
psychiatric symptoms and their response to treatment. Many types of mental health
profes-sionals and, in some cases, nonclinicians can be trained to ad-minister
these rating scales.
Although most practicing clinicians do not commonly
use structured instruments to assess or follow-up patients, a small number of
rating scales have come to be used routinely in clini-cal practice. For
example, the Abnormal Involuntary Movement Scale (Figure 19.3) is often used to
monitor patients receiving antipsychotic medication for the presence of tardive
dyskinesia, and the Global Assessment of Functioning Scale (Figure 19.4), which
is a slight modification of the Global Assessment Scale, is now used in Axis V
in the Diagnostic and Statistical Manual
of Mental Disorders, Fourth
Edition (DSM-IV-TR).
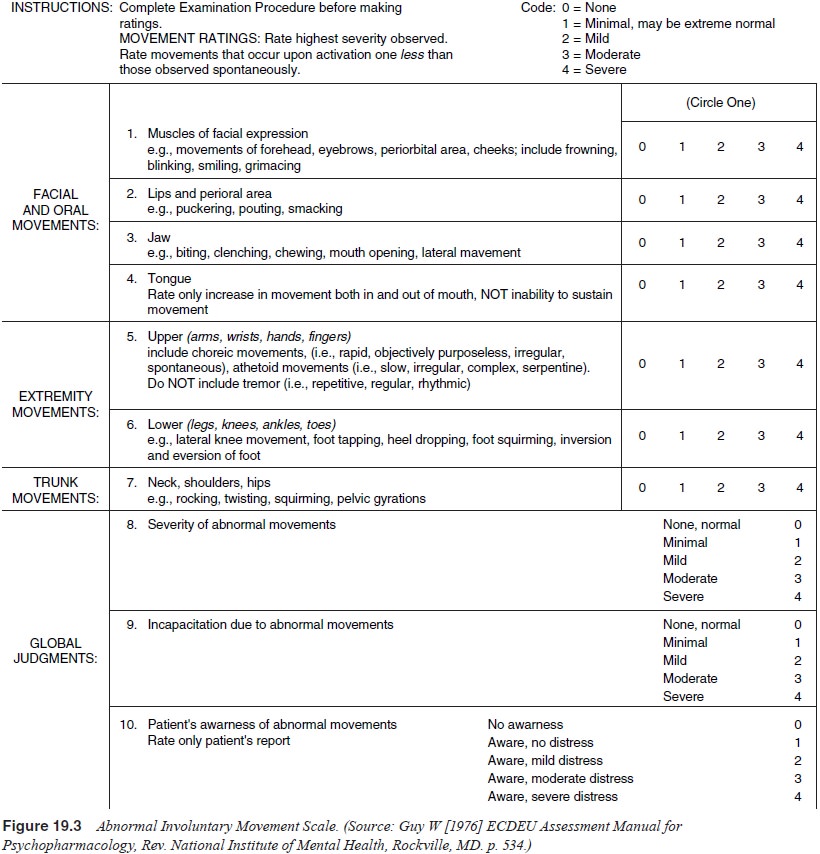
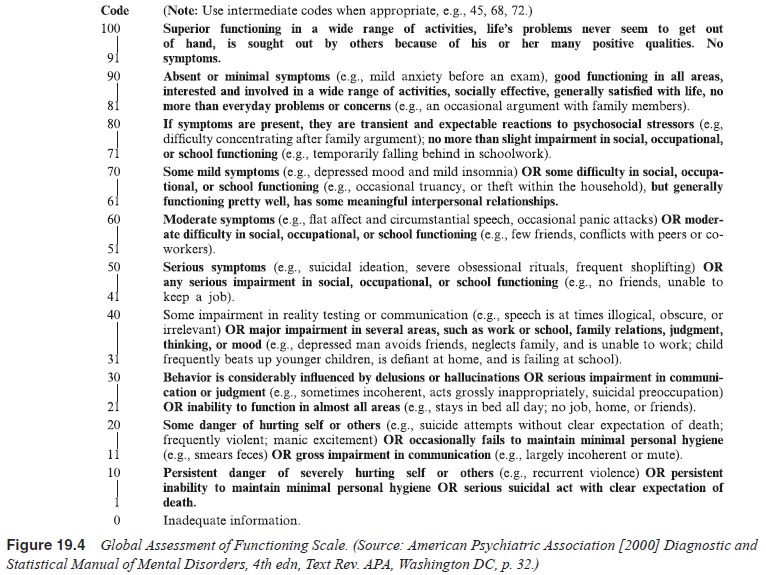
Table 19.11 shows some of the most commonly cited
struc-tured instruments and rating scales. Hundreds of other special-ized
scales are also in use to assess such diverse areas as person-ality disorder,
aggressive behavior, sexual practices, stressful life events and quality of
life.
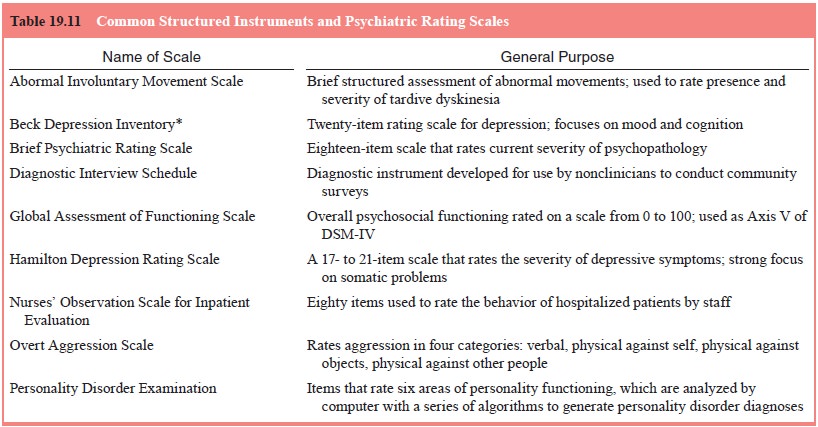
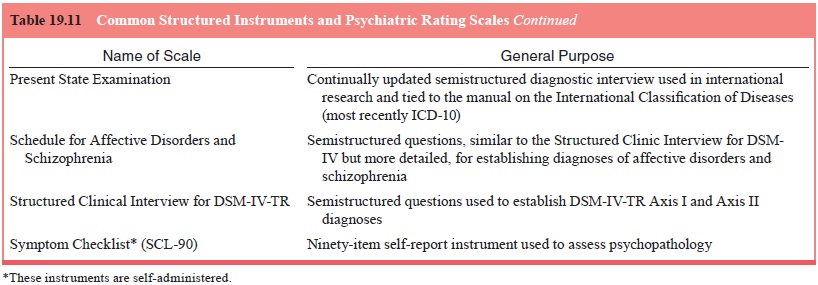
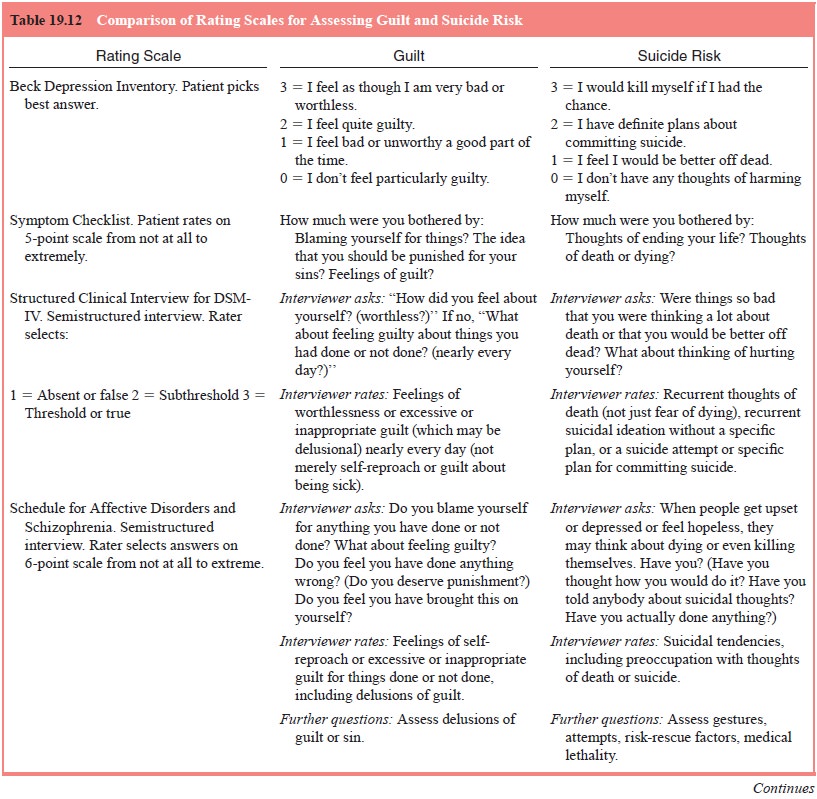
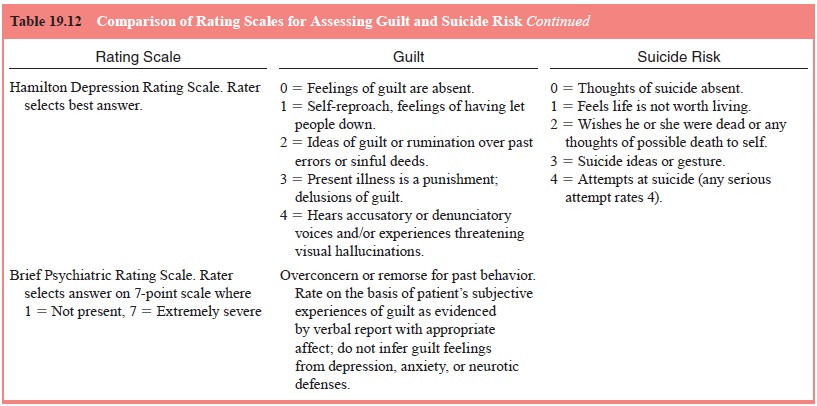
Table 19.12 gives an example of how these different
rat-ing scales approach the assessment of two symptoms: guilt, a purely
subjective state of mind, and suicide risk, an incli-nation that is assessed
using both subjective and behavioral components.
Related Topics