Chapter: Essentials of Psychiatry: Clinical Evaluation and Treatment Planning: A Multimodal Approach
Treatment Planning - Clinical Evaluation and Treatment Planning: A Multimodal Approach
Treatment Planning
The psychiatric evaluation is the basis for
developing the case formulation, initial treatment plan, initial disposition
and com-prehensive treatment plan.
Case Formulation
The case formulation is the summary statement of
the immediate problem, the context in which the problem has arisen, the
tenta-tive diagnosis and the assessment of risk. The latter two areas are
described next in more detail.
Assessment of Risk
The assessment of risk is the most crucial
component of the for-mulation because the safety of the patient, the clinician
and oth-ers is the foremost concern in any psychiatric evaluation. Four areas
are important: suicide risk, assault risk, life-threatening medical conditions
and external threat.
Suicide Risk
The risk of suicide is the most common
life-threatening situation mental health professionals encounter. Its
assessment is based on both an understanding of its epidemiology, which alerts
the clinician to potential danger, and the individualized assessment of the
patient. Suicide is the eighth leading cause of death in the USA. In the past
century, the rate of suicide has averaged 12.5 per 100 000 people. Studies of
adults and adolescents who commit suicide reveal that more than 90% of them
suffered from at least one psychiatric disorder and as many as 80% of them
consulted a physician in the months preceding the event. An astute risk
as-sessment therefore provides an opportunity for prevention.
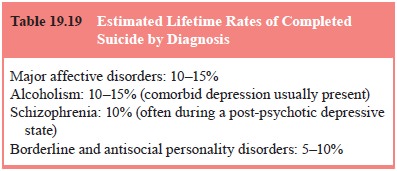
For those who complete suicide, the most common
diag-noses are affective disorder (45–70%) and alcoholism (25%). In certain
psychiatric disorders, there is a significant lifetime risk for suicide, as
listed in Table 19.18. Panic disorder is associated with an elevated rate of
suicidal ideation and suicide attempts but estimates of rates of completed
suicide are not well established.
Suicide rates increase with age, although rates
among young adults have been steadily rising. Women attempt suicide more often
than men, but men are three to four times more likely than women to complete
suicide. Whites have higher rates of sui-cide than other groups.
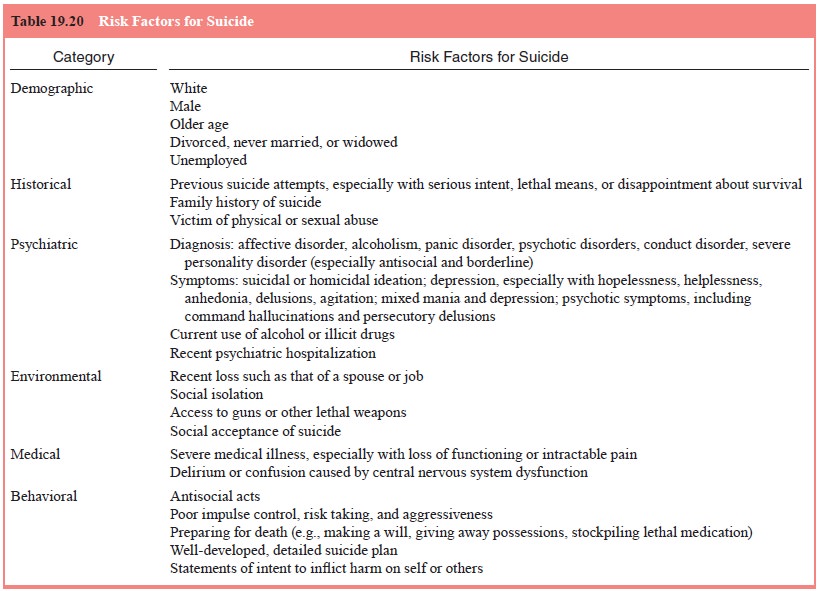
A patient may fit the diagnostic and demographic
profile for suicide risk, but even more essential is the individualized
assessment developed by integrating information
from all parts of the psychiatric evaluation. This includes material from the
present illness (e.g., symptoms of depression, paranoid ideation about being
harmed), past psychiatric history (e.g., prior attempts at suicide or other
violent behavior), personal history (e.g., recent loss), family history (e.g.,
suicide or violence in close relatives), medical history (e.g., presence of a
terminal illness) and the MSE (e.g., helplessness, suicidal ideation).
The most consistent predictor of future suicidal
behavior is a prior history of such behavior, which is especially worrisome
when previous suicide attempts have involved serious intent or lethal means.
Among the factors cited as having an association with risk of suicide are
current use of drugs and alcohol; recent loss, such as of a spouse or job;
social isolation; conduct disorders and antisocial behavior, especially in
young men; the presence of depression, especially when it is accompanied by
hopelessness, helplessness, delusions, or agitation; certain psychotic
symp-toms, such as command hallucinations and frightening paranoid delusions;
fantasies of reunion by death; and severe medical ill-ness, especially when it
is associated with loss of functioning, in-tractable pain, or central nervous
system dysfunction. Table 19.19 lists risk factors for suicide. It should be
noted that assisted sui-cide is now more openly discussed among people with terminal
illnesses and has gained some measure of acceptability. None-theless, the vast
majority of people who are bereaved or suffer from a serious medical illness do
not end their lives by suicide. Adequate end-of-life care should forestall
requests for assisted suicide. Although suicidal intent may be lacking,
patients who are delirious and confused as a result of a medical illness are
also at risk of self-injury.
It is essential to be clear about whether the
patient has pas-sive thoughts about suicide or actual intent. Is there a plan?
If so, how detailed is it, how lethal, and what are the chances of rescue? The
possession of firearms is particularly worrisome, because nearly two-thirds of
documented suicides among men and more than a third among women have involved
this method
Factors that may protect against suicide include
convictions in opposition to suicide; strong attachments to others, including
spouse and children; and evidence of good impulse control.
In addition to the assessment of risk factors, it
is important to decide whether the possibility of suicide is of immediate
con-cern or represents a long-term ongoing risk.
Risk of Assault
Unlike those who commit suicide, most people who
commit vio-lent acts have not been diagnosed with a mental illness, and data
clarifying the relationship between mental illness and violence are limited.
The most common psychiatric diagnoses associated with violence are
substance-related disorders. Conduct disorder and antisocial personality
disorder, by definition, involve aggres-sive, violent and/or unlawful behavior.
In the absence of comorbid substance-related
disorders, most people with such major mental illnesses as affective dis-orders
and schizophrenia are not violent. But data from the Na-tional Institute of
Mental Health Epidemiological Catchment Area Study suggest that these diagnoses
are associated with a higher rate of violence than that found among individuals
who have no diagnosable mental illness. The MacArthur Violence Risk Assessment
Study found this was only true for psychiatric patients with substance abuse
(Steadman et al., 1998).
Table 19.20 lists risk factors for violence. As
with suicide, the best predictor of future assault is a history of past
assaultInformation from the psychiatric evaluation that helps in this
as-sessment includes the present illness (e.g., preoccupation with vengeance,
especially when accompanied by a plan of action), psychiatric history (e.g.,
childhood conduct disorder), family his-tory (e.g., exposure as a child to
violent parental behavior), per-sonal history (e.g., arrest record), and the
MSE (e.g., homicidal ideation, severe agitation). Other predictors of violence
include possession of weapons and current illegal activities. There is
considerable overlap between risk factors for suicide and those for violence.
Life-threatening Medical Conditions
It is essential to consider life-threatening
medical illness as a po-tential cause of psychiatric disturbance. Clues to this
etiology can be found in the present illness (e.g., physical complaints),
family history (e.g., causes of death in close family members), medical history
(e.g., previous medical conditions and treatments), physi-cal examination
(e.g., abnormalities identified) and MSE (e.g., confusion, fluctuation in
levels of consciousness). Laboratory assessment, brain imaging and structured
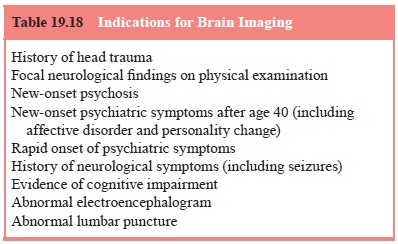
tests for neuropsychi-atric impairment may also be essential.
Probably the most common life-threatening medical sit-uations that the psychiatrist evaluates are acute central nerv-ous system changes caused by medical conditions and accom-panied by mental status alterations. These include increased intracranial pressure or other cerebral abnormalities, seve metabolic alterations, toxic states and alcohol withdrawal. Pa-tients may be at risk of death if these states are not quickly identified.
External Threat
Some patients who present for psychiatric
evaluation are at risk as a result of life-threatening external situations.
Such patients can include battered women, abused children and victims of
ca-tastrophes who lack proper food or shelter. Information about these
conditions is usually obtained from the present illness, the personal history
the medical history and physical examination.
Related Topics