Chapter: Essentials of Psychiatry: Clinical Evaluation and Treatment Planning: A Multimodal Approach
Physical Examination
Physical Examination
The physical examination is an important part of
the compre-hensive psychiatric evaluation for several reasons. First, many
patients who present with psychiatric symptoms may have under-lying medical
problems that are causing or exacerbating the pre-senting symptoms. For
example, an agitated, delirious patient may be septic or a patient being
treated for an autoimmune disorder who develops new onset paranoia may have a
steroid-induced

psychosis. Secondly, the patient’s physical
capacity to tolerate certain psychiatric medications, such as tricyclic
antidepressants or lithium, must be assessed. Finally, many patients who
present to a psychiatrist have had inadequate medical care and should be
routinely examined to assess their general level of physical health. This is
especially true for patients with chronic mental illness or substance abuse. In
some settings, such as emergency rooms and inpatient wards, the psychiatrist
may want to perform the physical examination; in others, it may be more
appropri-ate to refer the patient to a general practitioner for this purpose.
Genital, rectal and breast examinations can usually be included even for
anxious and paranoid patients, but when they must be postponed, care should be
taken to complete them at a later time. A same-sex chaperone is necessary for
the security of both the patient and the examiner
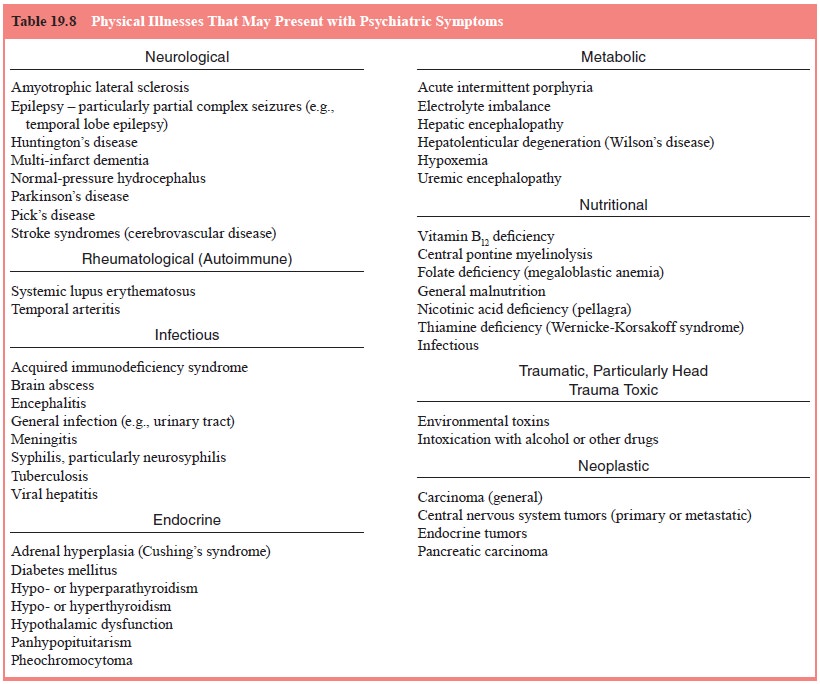
Certain
aspects of the information obtained in the psy-chiatric interview should alert
the psychiatrist to the need for a physical examination. Any indication (Table
19.7) from the his-tory that the psychiatric symptoms followed physical trauma,
in-fection, medical illness, or drug ingestion should prompt a full physical
examination. Similarly, the acute onset of psychiatric symptoms in a previously
psychiatrically healthy individual, as well as symptoms arising at an unusual
age, should raise ques-tions about potential medical causes (Table 19.8).
New-onset psychosis or mania in a previously
healthy 65-year-old is representative of a case requiring pursuit of a medical
condition as the cause because these disorders do not commonly present at this
age. Any gross physical abnormalities, such as gait disturbances, skin lesions,
eye movement abnormalities, lacera-tions, flushed skin, or drooling, should
raise the interviewer’s
suspicion that there might be an underlying medical
condition. Urinary or fecal incontinence is also highly suggestive of a
medi-cal etiology. Stigmata of drug or alcohol use or abuse, such as di-lated
or pinpoint pupils, track marks, evidence of skin popping, or frank evidence of
intoxication (e.g., alcohol on the breath) should also signal the need for a
more thorough physical examination. Abnormalities of speech, such as impaired
fluency or dysarthria, may indicate the presence of an underlying medical
disturbance. Many mood problems may be caused by physical disorders, and even
apparently healthy patients with dysthymia may have hy-pothyroidism that can be
treated medically. Finally, any cognitive disturbances, such as disorientation,
fluctuating level of alert-ness, inattentiveness, or memory problems are, until
proved oth-erwise, evidence of a physical problem that is causing psychiatric
symptoms. In such situations, careful attention should be paid to the patient’s
vital signs, neurological examination (See section on Neurological
Examination), and any indications of infection. In a hospital setting, a
physical examination, including a careful as-sessment of the patient’s vital
signs (including orthostatic meas-urements), cardiovascular status and
pulmonary status precedes the prescription of most psychiatric medications.
Psychiatrists should pay particular attention to a patient’s cardiovascular
status (e.g., electrocardiographic abnormalities, orthostatic hy-potension,
decreased cardiac ejection fraction) before beginning tricyclic
antidepressants, which may induce cardiac conduction disturbances and thus must
be used with caution for patients with such cardiac abnormalities as
arrhythmias or other con-duction abnormalities. Patients taking medications
such as low-potency neuroleptics, monoamine oxidase inhibitors and tricyclic
antidepressants should be assessed for orthostatic hypotension, especially if
they are elderly. If beta-blockers such as propranolol are being considered,
patients should be evaluated for the pres-ence of asthma, which may be
exacerbated by these drugs.
Physical examination may also be warranted during
treat-ment with medication if physical symptoms arise. For example, fever and a
change of mental status during a course of neurolep-tics require a full
physical and neurological examination to rule out neuroleptic malignant
syndrome. Urinary retention induced by medications with anticholinergic side
effects requires an abdominal examination to assess bladder fullness.
Anticholin-ergic-induced constipation may warrant abdominal or rectal
examination to assess for impaction. When patients are seen in office-based
practices, the psychiatrist most often obtains a care-ful medical history and
may complete simple procedures such as blood pressure checks but may refer the
patient to another physi-cian for a complete physical examination.
Related Topics