Chapter: Medical Physiology: Cardiac Output, Venous Return, and Their Regulation
Control of Cardiac Output by Venous Return-Role of the Frank-Starling Mechanism of the Heart
Control of Cardiac Output by Venous Return—Role of the Frank-Starling Mechanism of the Heart
When one states that cardiac output is controlled by venous return, this means that it is not the heart itself that is the primary controller of cardiac output.
Instead, it is the various factors of the peripheral cir-culation that affect flow of blood into the heart from the veins, called venous return, that are the primary controllers.
The main reason peripheral factors are usually more important than the heart itself in controlling cardiac output is that the heart has a built-in mechanism that normally allows it to pump automatically whatever amount of blood that flows into the right atrium from the veins. This mechanism, called the Frank-Starlinglaw of the heart. Basically,this law states that when increased quantities of blood flow into the heart, the increased blood stretches the walls of the heart chambers. As a result of the stretch, the cardiac muscle contracts with increased force, and this empties the extra blood that has entered from the systemic circulation. Therefore, the blood that flows into the heart is automatically pumped without delay into the aorta and flows again through the circulation.
Another important factor, is that stretching the heart causes the heart to pump faster—at an increased heart rate.That is, stretch of the sinus node in the wall of the right atrium has a directeffect on the rhythmicity of the node itself to increase heart rate as much as 10 to 15 per cent. In addition, the stretched right atrium initiates a nervous reflex called the Bainbridge reflex, passing first to the vaso-motor center of the brain and then back to the heart by way of the sympathetic nerves and vagi, also to increase the heart rate.
Under most normal unstressful conditions, thecardiac output is controlled almost entirely by periph-eral factors that determine venous return. However, we shall see later that if the returning blood does become more than the heart can pump, then the heart becomes the limiting factor that deter-mines cardiac output.
Cardiac Output Regulation Is the Sum of Blood Flow Regulation in All the Local Tissues of the Body—Tissue Metabolism Regulates Most Local Blood Flow
The venous return to the heart is the sum of all the local blood flows through all the individual tissue segments of the peripheral circulation. Therefore, it follows that cardiac output regulation is the sum of all the local blood flow regulations.
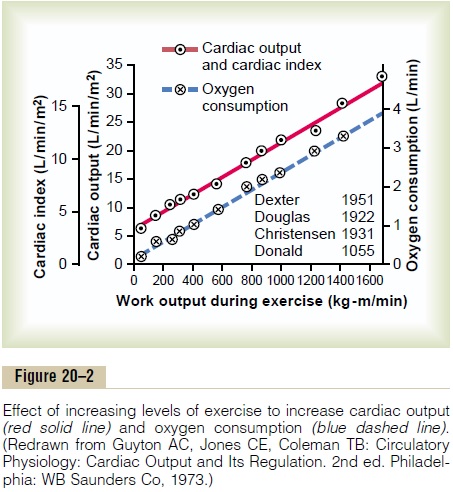
In most tissues, blood flow increases mainly in proportion to each tissue’s metab-olism. For instance, local blood flow almost always increases when tissue oxygen consumption increases; this effect is demonstrated in Figure 20–2 for different levels of exercise. Note that at each increasing level of work output during exercise, the oxygen consumption and the cardiac output increase in parallel to each other.
To summarize, cardiac output is determined by the sum of all the various factors throughout the body that control local blood flow. All the local blood flows summate to form the venous return, and the heart automatically pumps this returning blood back into the arteries to flow around the system again.
Effect of Total Peripheral Resistance on the Long-Term Cardiac Output Level. Figure 20–3 is the same as Figure 19–5.It is repeated here to illustrate an extremely important principle in cardiac output control: Under most normal conditions, the long-term cardiac output level varies reciprocally with changes in total peripheral resistance. Note in Figure 20–3 that when the total peripheral resistance is exactly normal (at the 100 per cent mark in the figure), the cardiac output is also normal. Then, when the total peripheral resistance increases above normal, the cardiac output falls; con-versely, when the total peripheral resistance decreases, the cardiac output increases. One can easily under-stand this by reconsidering one of the forms of Ohm’s law:
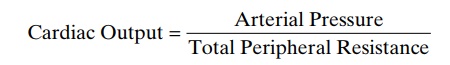
The meaning of this formula, and of Figure 20–3, is simply the following: Any time the long-term level of total peripheral resistance changes (but no other func-tions of the circulation change), the cardiac output changes quantitatively in exactly the opposite direction.
The Heart Has Limits for the Cardiac Output That It Can Achieve
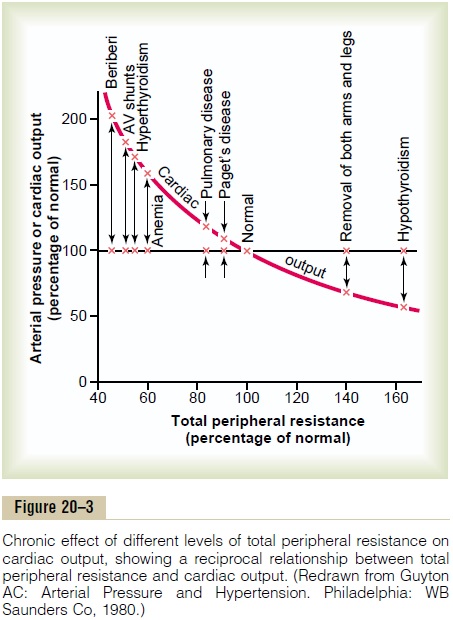
There are definite limits to the amount of blood that the heart can pump, which can be expressed quantita-tively in the form of cardiac output curves.
Figure 20–4 demonstrates the normal cardiac outputcurve, showing the cardiac output per minute at eachlevel of right atrial pressure. This is one type of cardiacfunction curve. Notethat the plateau level of this normal cardiac output curve is about 13 L/min, 2.5 times the normal cardiac output of about 5 L/min. This means that the normal human heart, functioning without any special stimula-tion, can pump an amount of venous return up to about 2.5 times the normal venous return before the heart becomes a limiting factor in the control of cardiac output.
Shown in Figure 20–4 are several other cardiac output curves for hearts that are not pumping nor- mally. The uppermost curves are for hypereffective hearts that are pumping better than normal. The low- ermost curves are for hypoeffective hearts that are pumping at levels below normal.
Factors That Can Cause Hypereffective Heart
Only two types of factors usually can make the heart a better pump than normal. They are (1) nervous stim-ulation and (2) hypertrophy of the heart muscle.
Effect of Nervous Excitation to Increase Heart Pumping. We saw that a combination of (1) sympa-thetic stimulation and (2) parasympathetic inhibition does two things to increase the pumping effectiveness of the heart: (1) it greatly increases the heart rate— sometimes, in young people, from the normal level of 72 beats/min up to 180 to 200 beats/min—and (2) it increases the strength of heart contraction (which is called increased “contractility”) to twice its normal strength. Combining these two effects, maximal nervous excitation of the heart can raise the plateau level of the cardiac output curve to almost twice the plateau of the normal curve, as shown by the 25-liter level of the uppermost curve in Figure 20–4.
Increased Pumping Effectiveness Caused by Heart Hypertrophy.
A long-term increased workload, but not so much excess load that it damages the heart, causes the heart muscle to increase in mass and contractile strength in the same way that heavy exercise causes skeletal muscles to hypertrophy. For instance, it is common for the hearts of marathon runners to be increased in mass by 50 to 75 per cent. This increases the plateau level of the cardiac output curve, sometimes 60 to 100 per cent, and therefore allows the heart to pump much greater than usual amounts of cardiac output.
When one combines nervous excitation of the heart and hypertrophy, as occurs in marathon runners, the total effect can allow the heart to pump as much 30 to 40 L/min, about 21/2 times normal; this increased level of pumping is one of the most important factors in determining the runner’s running time.
Factors That Cause a Hypoeffective Heart
Any factor that decreases the heart’s ability to pump blood causes hypoeffectivity. Some of the factors that can do this are the following:
Coronary artery blockage, causing a “heart attack”
Inhibition of nervous excitation of the heart Pathological factors that cause abnormal heart rhythm or rate of heartbeat Valvular heart disease
Increased arterial pressure against which the heart must pump, such as in hypertension
Congenital heart disease Myocarditis
Cardiac hypoxia
What Is the Role of the Nervous System in Controlling Cardiac Output?
Importance of the Nervous System in Maintaining the Arterial Pressure When the Venous Return and Cardiac Output Increase
Figure 20–5 shows an important difference in cardiac output control with and without a functioning auto-nomic nervous system. The solid curves demonstrate the effect in the normal dog of intense dilation of the peripheral blood vessels caused by administering the drug dinitrophenol, which increased the metabo-lism of virtually all tissues of the body about fourfold. Note that with nervous control to keep the arterial pressure from falling, dilating all the peripheral blood vessels caused almost no change in arterial pressure but increased the cardiac output almost fourfold.
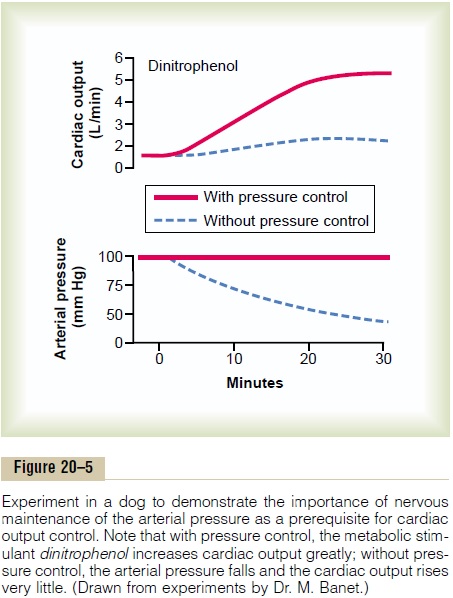
However, after autonomic control of the nervous system had been blocked, none of the normal circula-tory reflexes for maintaining the arterial pressure could function, and vasodilation of the vessels with dinitrophenol (dashed curves) then caused a profound fall in arterial pressure to about one half normal, and the cardiac output rose only 1.6-fold instead of 4-fold.
Thus, maintenance of a normal arterial pressure by the nervous reflexes, by mechanisms explained, is essential to achieve high cardiac outputs when the peripheral tissues dilate their vessels to increase the venous return.
Effect of the Nervous System to Increase the Arterial Pressure During Exercise. During exercise, intense increase inmetabolism in active skeletal muscles acts directly on the muscle arterioles to relax them and to allow ade-quate oxygen and other nutrients needed to sustain muscle contraction. Obviously, this greatly decreases the total peripheral resistance, which normally would decrease the arterial pressure also. However, the nervous system immediately compensates. The same brain activity that sends motor signals to the muscles sends simultaneous signals into the autonomic nervous centers of the brain to excite circulatory activity, causing large vein constriction, increased heart rate, and increased contractility of the heart. All these changes acting together increase the arterial pressure above normal, which in turn forces still more blood flow through the active muscles.
In summary, when local tissue vessels dilate and thereby increase venous return and cardiac output above normal, the nervous system plays an exceed-ingly important role in preventing the arterial pressure from falling to disastrously low levels. In fact, during exercise, the nervous system goes even further, pro-viding additional signals to raise the arterial pressure even above normal, which serves to increase the cardiac output an extra 30 to 100 per cent.
Related Topics