Chapter: Modern Medical Toxicology: Neurotoxic Poisons: Stimulants
Cocaine: Diagnosis, Treatment - Stimulant Neurotoxic Poisons
Diagnosis
Blood
or plasma cocaine levels are not clinically useful, although they may be
advisable to be done in medicolegal cases. Qualitative urine tests using kits
may be helpful in clinical diagnosis (by utilising chromatography,
radioim-munoassay, enzyme immunoassay, fluorescence polarisa-tion immunoassay,
and enzyme-multiplied immunoassay technique). Cocaine metabolites can be
identified in the urine and provide a method for qualitatively identifying
suspected cocaine poisoning or abuse. Benzoylecgonine, the major metabolite of
cocaine, can usually be detected in urine for 48 to 72 hours after cocaine use.
Other
Diagnostic Clues—
·
Hair analysis: Cocaine benzoylecgonine and
ecgoninemethyl ester can be analysed in hair samples by GC-MS and RIA. This can
be done in adults, as well as in any infant whose mother was a cocaine user. It
must be noted that external contamination of hair can occur from crack smoke,
but that can be washed off, whereas systemic exposure is not affected by
washing the hair.
·
ECG: Non-Q-wave myocardial infarction,
with thepresence of a Twave infarct ECG pattern is often seen in cocaine users.
During acute cocaine use abnormalities are more prevalent, and the QT interval
is prolonged. Two-dimensional echocardiography may be useful in detecting the
presence of new regional wall-motion abnormalities in patients experiencing
cocaine-induced chest pain. Troponin levels may be more useful in evalu-ating
potential myocardial injury than creatinine kinase.
·
Acid-base abnormalities: Arterial blood gases incocaine
abusers show a pH varying from 7.35 to 7.5. Alkalosis (pH > 7.45) is caused
by hyperventilation, and is manifested by tachypnoea and low PaCO2.
About one third of patients show evidence of acidosis which may be the result
of hypoventilation secondary to depressed mental status or chest trauma.
Metabolic acidosis is not uncommon, and usually results from convulsions,
agitation, or trauma.
·
Estimate serum creatine kinase for evidence of rhab-domyolysis.
Monitor renal function and urine output in patients with elevated CPK.
·
X-ray: Body packer syndrome can bediagnosed by plain films of the abdomen
in the supine and upright positions. However, false negatives have been
reported. Radiography may not detect cellophane-wrapped packets or crack vials.
Even false-negative abdominal CT scans have been reported. It is therefore
advisable to perform a contrast study of the bowel withfollow-up X-rays 5 hours
after the oral ingestion of a water-soluble contrast compound such as meglumine
amidotrizoate (50 ml). Daily views are performed there-after until negative
views coincide with the passage of two drug packet-free stools.
![]()
Treatment
Acute Poisoning:
Activated
charcoal adsorbs cocaine in vitro under both acidic and alkaline conditions,
and can be administered in cases of ingestion.
Hyperthermia—
o
Minimise physical activity and sedate with benzo-diazepines.
o
Ice baths, packs, cool water with fans, etc.
o
Oxygen D50W (as necessary).
o
Diazepam 5 mg IV or lorazepam 2–4 mg IV titrated to effect.
o
Paracetamol 2000 mg (in the form of 500 mg rectal
suppositories).
o
Severe, intractable cases may respond to dantrolene (1
mg/kg) every 6 hours. Alternatively, bromocrip-tine can be administered orally
in a nasogastric tube.
Anxiety
and agitation—
·
Diazepam 5–10 mg IV, or lorazepam
2–4 mg IV titrated to effect.
·
Physical restraints.
·
Antipsychotics such as haloperidol
or droperidol, and phenothiazines are not recommended since they can induce
malignant hyperthermia and convul-sions.
Convulsions—
·
Diazepam 5–10 mg IV, or lorazepam 2–4 mg IV titrated to
effect.
·
Phenobarbitone 25–50 mg/min up to 10–20 mg/kg.
·
If seizures are not controlled by the above measures,
consider continuous infusion of midazolam (0.2 mg/ kg slow bolus, or 0.75 to 10
mcg/kg/min as infu-sion), or propofol (1 to 2 mg/kg, followed by 2 to 10
mg/kg/hr) or pentobarbitone (10 to 15 mg/kg at a rate of 50 mg/min, followed by
0.5 to 1 mg/kg/hr).
·
Intractable convulsions may require neuromuscular paralysis
with intubation and mechanical ventila-tion.
·
Cerebrovascular accidents—Neurosurgical consultation is
mandatory.
Hypertension—
Without
tachycardia:
--
Phentolamine 0.02 to 0.1 mg/kg IV -- Nifedipine 0.1 to 0.2 mg/kg IV
-- Nitroprusside 2 to 10 mcg/kg/min IV.
With
tachycardia:
--
Labetolol 10 to 20 mg IV, repeated every 10 minutes (max: 300 mg). Labetolol
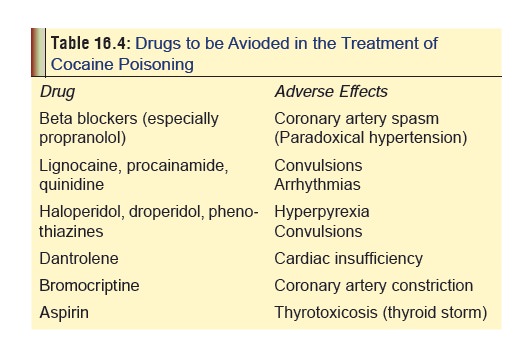
must be used with caution (Table 16.4).
-- Nitroglycerine IV titrated to effect.
With
chest pain:
-- Nitroglycerine drip.
-- Oxygen by nasal cannula (5 L/min).
-- Monitor cardiac status.
--
If systolic BP is higher than 120 mmHg, admin-ister nitroglycerine sublingually
(up to 3 tablets or 3 sprays of 0.4 mg each).
-- If pain does not respond to
nitroglycerine, use morphine (2 mg IV titrated to pain relief).
--
Obtain ECG.
--
If chest pain is strongly suggestive of a myocar-dial infarction,
consider thrombolytic therapy.
-- Diazepam 5 mg IV, or lorazepam
2–4 mg IV titrated to effect can prevent excess production of catecholamines by
the CNS.
--
Mechanical reperfusion (angioplasty).
Arrhythmias—
Sinus tachycardia:
-- Observation. -- Oxygen.
--
D50W (as necessary).
-- Diazepam 5–10 mg IV, or lorazepam
2–4 mg IV titrated to effect (if indicated).
Supraventricular tachycardia:
-- Observation -- Oxygen
--
D50W ( as neccesary).
-- Diltiazem 20 mg IV, or verapamil
5 mg IV. -- Adenosine 6–12 mg IV for AV node re-entry.
--
Cardioversion (if necessary).
Ventricular arrhythmias:
--
Obtain an ECG, institute continuous cardiac monitoring and administer
oxygen. Evaluate for hypoxia, acidosis, and electrolyte disorders (particularly
hypokalaemia, hypocalcaemia, and hypomagnesaemia).
--
Oxygen.
--
D50W ( as necessary).
--
Hypertonic sodium bicarbonate: Sodium bicarbonate may be useful in the
treatment of QRS widening and ventricular arrhythmias associated with acute
cocaine use. A reasonable starting dose is 1 to 2 mEq/kg repeated as needed.
Monitor arterial blood gases, maintain pH 7.45 to 7.55.
-- Diazepam 5 mg IV, or lorazepam
2–4 mg IV. -- Lignocaine 1.5 mg/kg IV bolus, followed by 2 mg/min infusion.
Watch out for adverse effects (Table
16.4). Procainamide may also be used with caution.
--Defibrillation (if
haemodynamically unstable).
Myocardial infarction—
IV line.
Oxygen.
Aspirin to inhibit platelet
aggregation. Watch out for increased thyroxine levels (Table 16.4).
For systolic BP higher than 100
mmHg, admin-ister sublingual nitroglycerine or nifedipine 10 mg orally, or
phentolamine 1 to 5 mg IV (followed by a drip of 10 mg in 1 litre of D5W
at 10 ml/min).
For life-threatening arrhythmias,
use of type IA antiarrhythmic agents may be considered (with caution).
Thrombolytic therapy may be
necessary if myocar-dial infarction is not amenable to relief by nitrates, calcium
channel blockers, or phentolamine. Caution about the use of thrombolytics in
cocaine-associ-ated acute myocardial infarction (AMI) is generally advocated.
Thrombolytics should be avoided in patients with cocaine-induced myocardial
infarc-tion and uncontrolled hypertension, because of the increased risk of
intracranial haemorrhage.
Aortic dissection—The hypertension
that precipitated aortic dissection must be controlled immediately with
nitroprusside and calcium channel blockers.
Pulmonary oedema—
·
Frusemide 20–40 mg IV.
·
Morphine sulfate 2 mg IV titrated to pain relief.
·
Nitroglycerine drip titrated to blood pressure or
respiratory status.
·
Phentolamine or nitroprusside (if necessary).
·
Incubate and ventilate.
·
Monitor fluids with pulmonary artery catheter.
Rhabdomyolysis—
·
Cardiac monitoring.
·
Serial potassium determinations.
·
Serial serum creatine kinase and urine myoglobin studies.
·
IV hydration (urine output must be maintained at 3
ml/kg/hr).
·
Dopamine and frusemide (60 mg three times a day) may reduce
renal vascular resistance and help in reducing the number of haemodialyses
required to reverse oliguria.
Acidosis—Correction
of acidaemia through supportive care measures such as hyperventilation,
sedation, active cooling, and sodium bicarbonate infusion can have beneficial
effects on conduction defects.
Elimination enhancement measures—
·
Cocaine is rapidly metabolised. Forced diuresis, urine
acidification, dialysis, and haemoperfusion are ineffective in significantly
altering elimination.
·
Increasing the level of butyrylcholinesterase in the blood
(which metabolises cocaine to inactive compounds) could help in rapidly
inactivating cocaine in acute intoxications.
Chronic Poisoning:
a.
Psychotherapy—This involves cognitive-behavioural,
psychodynamic, and general supportive techniques. One example of a
cognitive-behavioural method uses contingency contracting, in which it is
agreed in advance that for a specified period of time (e.g. 3 months), if the
patient uses cocaine (as detected by supervised urine
testing), the therapist will initiate
b.
action that will result in serious
adverse consequences for the patient, such as informing the employer.
i. Interpersonal group therapy focuses on relation- ships,
and uses the group interactions to illustrate the interpersonal causes of
individual distress, and
ii. Modified dynamic group therapy is concerned with
emphasising character as it manifests itself individually and intrapsychically,
and in the context of interpersonal relationships with a focus on affect, of
interpersonal relationships with a focus on affect, self-esteem, and self-care.
c.
Group counselling—The most widely
used form of psychosocial treatment for cocaine dependence is group
counselling, in which the group is open-ended with rolling admissions; the
group leaders are drug counsel- lors, many of whom are recovering from
addiction, and the emphasis is on providing a supportive atmosphere, discussing
problems in recovery, and encouraging participation in multistep programmes.
d.
Pharmacotherapy—
·
Several drugs have been tried to
help ameliorate the manifestations of cocaine withdrawal. Many of these
(fenfluramine, trazodone, neuroleptic agents, etc.) have either not
demonstrated clinical efficacy, or have produced serious side effects.
·
Bromocriptine has successfully
reduced cocaine craving and decreased withdrawal symptoms in several studies.
Oral doses of 0.625 mg given 4 times daily may produce a rapid decrease in
psychi-atric symptoms. Dose can be decreased in patients experiencing adverse
effects.
·
Amantadine, a dopamimetic agent,
increases dopaminergic transmission and has been found to be useful in the
treatment of early withdrawal symptoms and short-term abstinence. The usual
dose recommended is 200 mg to 400 mg orally, daily, for up to 12 days. It is
probably as effective as bromocriptine, and less toxic.
·
Tricyclic antidepressants may be
useful for selected cocaine users with comorbid depression or intranasal use.
·
Initial studies with fluoxetine
promised good results, but craving actually worsened in some patients. Several studies
indicated better efficacy with carbamazepine for controlling craving.
Carbamazepine at doses of 200 to 800 mg orally, 2 to 4 times daily has
benefited some patients. Phenytoin also shows promise in helping to sustain
abstinence from cocaine in some patients.![]()
Related Topics