Chapter: Essentials of Psychiatry: Sleep and Sleep-Wake Disorders
Breathing-related Sleep Disorder
Breathing-related
Sleep Disorder
The
essential feature of this disorder is sleep disruption result-ing from sleep
apnea or alveolar hypoventilation, leading to com-plaints of insomnia or, more
commonly, excessive sleepiness. The disorder is not accounted for by other
medical or psychiatric disorders or by medications or other substances.
Diagnosis
The major
diagnostic criterion for sleep apnea is cessation of breathing lasting at least
10 seconds and an apnea index (number of apneic events per hour of sleep) of
five or more. Most apneic episodes are terminated by transient arousals.
Hypopneas (50% decrease in respiration) may also produce arousal or hypoxia
even when complete apneas do not occur. Therefore, rather than just the apnea
index, a respiratory disturbance index (number of respira-tory events, or
number of apneas plus hypopneas per hour of sleep) is used. Whereas the
criterion for the respiratory disturbance in-dex has not been fully
established, many psychiatrists use a respi-ratory disturbance index of 10 or
greater for purposes of diagnosis. Each time respiration ceases, the individual
must awaken to start breathing again. Once the person goes back to sleep,
breathing stops again. This pattern continues throughout the night.
Clini-cally, however, it is not unusual to see patients who stop breathing for
60 to 120 seconds with each event and experience hundreds of events per night.
Many individuals with BRSD cannot sleep and breathe at the same time and
therefore spend most of the night not breathing and not sleeping. In contrast,
the central alveolar hypoventilation syndrome is not associated with either
apneas or hypopneas, but impaired ventilatory control or hypoventilation
re-sults in hypoxemia. It is most common in morbid obesity.
Sleep apnea is characterized by repetitive episodes of upper airway obstruction that occur during sleep, resulting in numer-ous interruptions of sleep continuity, hypoxemia, hypercapnia, bradytachycardia, and pulmonary and systemic hypertension. It may be associated with snoring, morning headaches, dry mouth on awakening, excessive movements during the night, falling out of bed, enuresis, cognitive decline and personality changes, and complaints of either insomnia or, more frequently, hypersomnia and excessive daytime sleepiness. The typical patient with clini-cal sleep apnea is a middle-aged man who is overweight or who has anatomical conditions narrowing his upper airway.
There are three types of apnea. The first is
obstructive sleep apnea, which involves the collapse of the pharyngeal airway
during inspiration, with partial or complete blockage of airflow. The person
still attempts to breathe, and one can observe the diaphragm moving, but the
airway is blocked and therefore there is no air exchange. It can be caused by
baggi-ness or excessive pharyngeal mucosa and a large uvula, fatty infiltration
at the base of the tongue, or collapse of the pharyn-geal walls. The resulting
decreased air passage compromises alveolar ventilation and causes blood-oxygen
desaturation and strenuous attempts at inspiration through the narrowed airway,
all of which lighten and disrupt sleep. Hypercapnia, which re-sults either from
obstructive sleep apnea or from lung disease, reduces breathing without the
presence of disruptive inspira-tory efforts.
The
second type is central sleep apnea, which results from failure of the respiratory
neurons to activate the phrenic and inter-costal motor neurons that mediate
respiratory movements. There is no attempt to breathe, and although the airway
is not collapsed, there is no respiration. This type of apnea is more commonly
as-sociated with heart disease. The third type is mixed sleep apnea, which is a
combination, generally beginning with a central com-ponent and ending with an
obstructive component.
The
lifetime prevalence of BRSD in adults has been esti-mated to be 9% in men and
4% in women. The prevalence does increase with age, particularly in
postmenopausal women. The prevalence in the elderly has been estimated to be
28% in men and 19% in women.
During
apneas and hypopneas, the blood-oxygen level often drops to precarious levels.
In addition, one often sees car-diac arrhythmias and nocturnal hypertension in
association with the respiratory disturbances. The cardiac arrhythmias include
bradycardia during the events and tachycardia after the end of the events. It
is not unusual to see premature ventricular contractions, trigeminy and
bigeminy, asystole, second-degree atrioventricular block, atrial tachycardia,
sinus bradycardia and ventricular tach-ycardia. However, the electrocardiogram
taken during the wak-ing state might be normal. It is only during the
respiratory events during sleep that the abnormalities appear
BRSD,
especially central sleep apnea, is commonly seen in patients with congestive
heart failure. Cor pulmonale may also be a consequence of longstanding BRSD and
is seen in both sleep apnea syndrome and primary hypoventilation. Patients may
present with unexplained respiratory failure, polycythemia, right ventricular
failure and nocturnal hypertension. About 50% of patients with BRSD have
hypertension, and about one-third of all hypertensive patients have BRSD. In
the large cross-sectional study, it was found that both systolic and diastolic
blood pressure (SDB) as well as the prevalence of hypertension increased
signifi-cantly with increasing SDB (Nieto et
al., 2000). It has also been shown that there is a dose–response
association between SDB at baseline and hypertension 4 years later suggesting
that SDB may be a risk factor for hypertension and consequent cardiovascular
morbidity.
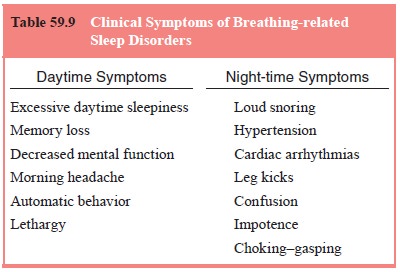
The most
common symptoms of BRSD include excessive daytime sleepiness and snoring. The
excessive daytime sleepi-ness probably results from sleep fragmentation caused
by the fre-quent nocturnal arousals occurring at the end of the apneas and
possibly from hypoxemia. The excessive daytime sleepiness is associated with
lethargy, poor concentration, decreased motiva-tion and performance, and
inappropriate and inadvertent attacks of sleep. Sometimes the patients do not
realize they have fallen asleep until they awaken.
The
second complaint is loud snoring, sometimes noisy enough to be heard throughout
or even outside the house. Of-ten the wife has complained for years about the
snoring and has threatened to sleep elsewhere if she has not moved out already.
Bed partners describe a characteristic pattern of loud snoring interrupted by
periods of silence, which are then terminated by snorting sounds. Snoring
results from a partial narrowing of the airway caused by multiple factors, such
as inadequate muscle tone, large tonsils and adenoids, long soft palate,
flaccid tissue, acromegaly, hypothyroidism, or congenital narrowing of the oral
pharynx. Snoring has been implicated not only in sleep ap-nea but also in
angina pectoris, stroke, ischemic heart disease and cerebral infarction, even
in the absence of complete sleep apneas. Because the prevalence of snoring
increases with age, especially in women, and because snoring can have serious
medi-cal consequences, the psychiatrist must give serious attention to
complaints of loud snoring. Snoring is not always a symptom of BRSD.
Approximately 25% of men and 15% of women are ha-bitual snorers.
Patients
with BRSD are frequently overweight. In some patients, a weight gain of 20 to
30 lb might bring on episodes of BRSD. The same fatty tissue seen on the
outside is also present on the inside, making the airway even more narrow.
Because obstructive sleep apnea is always caused by the collapse of the airway,
in patients of normal weight, anatomical abnormalities (such as large tonsils,
long uvula) must be considered.
Other
symptoms of BRSD include unexplained morning headaches, nocturnal confusion,
automatic behavior, dysfunction of the autonomic nervous system, or night
sweats. The severity of BRSD will depend on the severity of the cardiac
arrhythmias, hypertension, excessive daytime sleepiness, respiratory
distur-bance index, amount of sleep fragmentation and amount of oxy-gen
desaturation.
Mild to moderate sleep-related breathing
disturbances in-crease with age, even in elderly subjects without major
complaints about their sleep. The frequency is higher in men than in women, at
least until the age of menopause, after which the rate in women increases and
may approach that of men. With use of the apnea index of five or more apneic
episodes per hour as a cutoff crite-rion, prevalence rates range from 27 to 75%
for older men and from 0 to 32% for older women. In general, the severity of
apnea in these older persons is mild (an average apnea index of about 13) compared
with that seen in patients with clinical sleep ap-nea. However, older men and
women with mild apnea have been reported to fall asleep at inappropriate times
significantly more often than older persons without apnea. Furthermore, the
fre-quency of sleep apnea and other BRSDs is higher in individuals with hypertension,
congestive heart failure, obesity, dementia and other medical conditions.
Increased
mortality rates have been noted in excessively long sleepers, therefore sleep
apnea may account for some of these excess deaths. This is also consistent with
evidence that excess deaths from all causes increase between 2 and 8 AM,
specifically deaths related to ischemic heart disease in patients older than 65
years. There have been several studies suggest-ing that untreated sleep apnea
in the elderly may lead to shorter survival.
The
clinical significance of relatively mild “subclinical” sleep apneas is not
fully understood yet. Psychiatrists should be aware, however, that such
disturbances might be associated with either insomnia or excessive daytime
sleepiness. Furthermore, for some patients with sleep apnea, administration of
hypnotics, alcohol, or other sedating medications is relatively
contraindi-cated. The risk is not yet known, but reports indicate that
benzo-diazepines as well as alcohol may increase the severity of mild sleep
apnea. Therefore, psychiatrists should inquire about snor-ing, gasping, and
other signs and symptoms of sleep apnea before administering a sleeping pill.
If patients have excessive sleepi-ness or morning hangover effects while taking
benzodiazepines, major tranquilizers, or other sedating medications, the
psychia-trist should consider the possibility of an iatrogenic BRSD due to
medications.
The
diagnosis of BRSD must be differentiated from other disorders of excessive
sleepiness such as narcolepsy (Table 59.9). Patients with BRSD will not have
cataplexy, sleep-onset paraly-sis, or sleep-onset hallucination. Narcolepsy is
not usually as-sociated with loud snoring or sleep apneas. In laboratory
record-ings, patients with BRSD do not usually have sleep-onset REM periods
either at night or in multiple naps on the Multiple Sleep Latency Test.
However, one must be aware that both BRSD and narcolepsy can be found in the
same patient. BRSD must also be distinguished from other hypersomnias, such as
those related to major depressive disorder or circadian rhythm disturbances.
Treatment of Sleep Apnea
Sleep
apnea is sometimes alleviated by weight loss, avoidance of sedatives, use of
tongue-retaining devices and breathing air under positive pressure through a
face mask (continuous positive airway pressure [CPAP]). Oxygen breathed at
night may alleviate insomnia associated with apnea that is not accompanied by
im-peded inspiration. Surgery may be helpful, for example, to cor-rect enlarged
tonsils, a long uvula, a short mandible, or morbid obesity. Pharyngoplasty,
which tightens the pharyngeal mucosa and may also reduce the size of the uvula,
or the use of a cervical collar to extend the neck, may relieve heavy snoring. Although
tricyclic antidepressants are sometimes used in the treatment of clinical sleep
apnea in young adults, they may cause considerable toxic effects in older
people. The newer shorter-acting nonbenzo-diazepine hypnotics seem to be safer
in these patients and may be considered in those patients who snore.
Related Topics