Chapter: Essentials of Psychiatry: Childhood Disorders: The Autism Spectrum Disorders
Autism Spectrum Disorders: Treatment
Treatment
Nonpharmacological and Behavioral Treatments
Developing a comprehensive individual intervention
program for a child with ASD is a daunting task for the child’s parents (Figure
27.1). Each child is unique, with a different set of diffi-culties, as well as
strengths. The child’s primary physician must work with the parents to help
make this task less overwhelming. The physician can anticipate being asked
about a wide array of al-ternative treatments being offered in the community,
which vary enormously in their claims, in the integrity of those making the
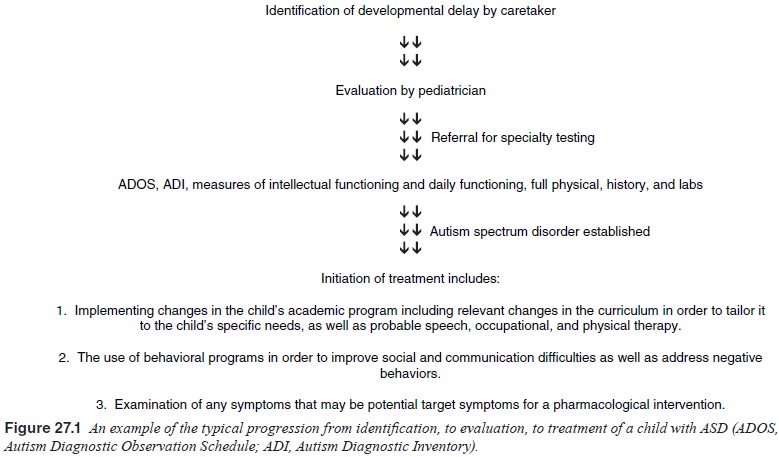
claims, and in their ultimate safety and utility.
The physician who immediately and outright and pejoratively dismisses these
alterna-tives as useless is not helpful to the child or his family (the
excep-tion being dangerous or cost-prohibitive prospective treatments). Rather,
it is helpful to listen and then educate the family, at a level commensurate
with their sophistication, about how to analyze and interpret claims and
science underlying these treatments.
Autistic disorder is recognized as a chronic
disorder with a changing course requiring a long-term course of treatment that
includes the necessity of an intervention with various treatments at different
times. At the present time, most treatments for the ASDs are symptom directed.
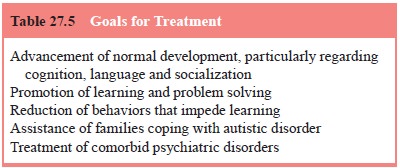
Given that there is no current cure for autistic disorder or the other ASD,
goals of treatment should encompass short-term and long-term needs of the
individual and his or her family (Table 27.5).
Every attempt should be made to achieve treatment
goals on a community-based environment since institutionalization may hinder a
child’s ability to learn means of functioning and adapting in typical social
settings. Community-based treatment can usually be maintained, except in times
of extreme stress or need, during which time a child (and family) might benefit
from respite care or brief hospitalization. Effective treatment often entails
setting appropriate expectations for the child and adjust-ing the child’s
environment to foster success.
Approach to Treatment
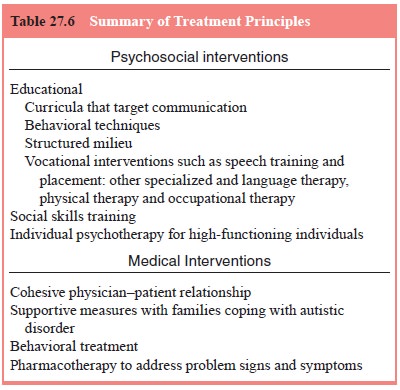
Because the autistic individual often requires
diverse treatments and services simultaneously, the role of the primary
physician is to be the coordinator of services. Frequent visits with the child
and the child’s caretakers initially allow the physician to assess the
in-dividual needs of the child while establishing a therapeutic alli-ance. An
effective approach often calls for the services of a number of professionals
working in a multidisciplinary fashion. This group may include psychiatrists,
pediatricians, pediatric neurologists, psychologists, special educators, speech
and language therapists social workers, and other specialized therapists (Table
27.6)
There is significant controversy over what
particular forms of therapy are best for children with ASD. Some of this
contro-versy is a result of claims of children making dramatic improve-ments
with some of these therapies.
The most successful interventions use a variety of
posi-tive reinforcement schedules to enhance the desired behaviors and
extinguish undesirable behaviors. Discrete trial training, an operant
conditioning model, is particularly useful in this regard. Generalization of
skills from the behavioral training environment to other settings is a key to
success. Applied behavioral analysis (ABA) uses careful assessment of adaptive
and maladaptive be-haviors and specific interventions addressing each behavior
and children receiving ABA have shown significant improvement in a number of
areas, including IQ, visual–spatial skills, language, and academics (Smith et al. 2001).
Problem Behaviors
A prerequisite to putting a behavioral plan in
place with a child with ASD is to identify the problem behaviors. These
behaviors often include interfering repetitive actions, self-injurious
behav-iors, or aggression. While there is little difficulty in identifying
these highly visible behaviors, what is much more difficult is 1) determining
the antecedents to these behaviors and 2) knowing what constitutes an
appropriate reaction or consequence to these behaviors on the part of the
caregiver.
To determine the antecedent is often
extraordinarily difficult, since it is often not apparent exactly what happened
in the environment that stimulated the behavior. This is particularly true if
the behavior is chronic and has developed some autonomous function (i.e., no
longer a stimulus–response event). To make things more complicated, it could be
internal perception or meaning of what happened in a child with autism (poor
language and socially nonresponsive) that may have initiated the behavior. For
example, imagine a nonverbal child frustrated by his inability to continue a
mental routine created by a teacher insisting that the child orient himself to
a school task like sitting in reading circle. Further, assume that the child
does not have a repertoire of appropriate social responses, and instead
responds by biting the teacher on the arm. It will be very difficult for the
teacher to know that the child was in the middle of a mental routine and not
able to communicate his distress verbally, thus leading to the inappropriate
behavior. It takes time and attention to understand these events processes in
children with ASD. Once they are clear, appropriate behavioral intervention is
possible.
Durand and Carr (1991) attempted to determine the
func-tion of problem behaviors in children with ASD. They concluded that most
behaviors could be classified as:
1. a need for help;
2. a desire to escape a stressful situation;
3. a desire to obtain an object;
4. an attempt to protest unwanted events;
5. an attempt to obtain stimulation or attention.
Obsessions and Rituals
Children with ASD often engage in rituals and
routines which appear to be an attempt to relieve anxiety and/or to exert
control over their environment. The key to success is a gradual shap-ing of the
behavior rather than dramatic expectations and harsh consequences. One should
begin intervention by evaluating pos-sible, underlying stimuli or predisposing
factors for the behavior. Strategies include determining when, where and for
how long an activity can take place. Additional strategies include making
environmental changes that reduce anxiety and even ignoring behaviors that do
not create undue problems. Adjunct pharmaco-logical intervention is often
helpful.
Communication Therapy
Up to 50% of children with ASD will not acquire
useful language. For those with some but not fully intact language skills,
speech therapy is an important part of therapeutic and academic plan-ning. An
emphasis on the social use of language is often helpful, and when the child can
articulate some of his or her needs, there is often a reduction in problem
behaviors.
Longitudinal studies indicate that children who
have not acquired useful language by the age of 7 usually have longstanding
verbal communication difficulties. For these children, it is often helpful to
devise an alternative means of communication: sign language or use of
augmentative communication devices such as computers and picture exchange
communication systems or PECS. PECS involves the use of photographs or line
drawings on cards. The child then points to or hands the appropriate card or
cards to another person in order to effect communication. Once again, children
are encouraged to use verbalization, when possible, in conjunction with sharing
the cards (Erdmann et al., 1996).
Irrespective of the technique used, establishing a consistent method of communication is central to the treatment of
individuals with ASD.
Social Interaction Therapy
Children and adults with ASD lack many of the
innate and learned social skills, especially reciprocal social interactions,
that most people simply take for granted. Maintaining appropri-ate
interpersonal distance, spontaneously initiating conversation, participating in
reciprocal social exchange and other facets of complex social interaction are
not easily incorporated in the rou-tine behaviors and activities of individuals
with ASDs. Subtlety and changing complexity of social interaction as well as
the in-nateness of many social skills is a central part of daily life and a key
to successful adaptation for typically functioning individu-als. Helping
individuals with ASDs address these challenges is difficult but also critical
for enhancing overall functioning.
Odom and Strain (1986) identified the three primary
techniques that can be effectively utilized:
· Proximity.
Establish proximity refers to the fact that it is very helpful to have the
child with ASD near other children in the en-vironment. The mere proximity
increases the likelihood of in-teraction and imitation as well as positive
social reinforcement.
·
Use. The use of prompts relates to have specific
prompts and reinforcement cues to use previously learned behaviors in so-cial
settings (e.g., “Raise your hand if you have a question”). Attention to
reinforcement means that even a less than fully competent attempt at
appropriate social behavior, even if re-sponse to a prompt, receive clear and
effective reinforcement when it occurs (e.g., calling on the child promptly
when he raises his hand to ask a question and also saying “You did a good job
when you raised your hand to ask the question”).
· Encourage
peer initiation is helpful to train peers who are likely to interact with the
child or adult with ASD in tech-niques for initiating social contact. For many
individuals, this means explaining the disability and dealing with fears or
bi-ases. For others, it may mean encouraging them to persist in their attempts
at engagement, even in the face of limited, inap-propriate, or inadequate
responses.
Academic Needs
Academic resources and placement are important
components in the child’s overall treatment. First and foremost, schools are
where children go to acquire social skills and acquaintances, as well as
academic skills. Secondly, schools often have a variety of skilled
professionals who are trained to provide necessary serv-ices for the individual
with ASD. And, finally, in the USA, all public schools have a statutory
obligation to provide all children (even those with disabilities) with a free
and appropriate educa-tion in the least restrictive environment.
Previously, children with ASD had been put in
alternative settings, but more recently there has been increased interest in
maintaining many ASD children in regular classroom settings. Studies seem to
indicate that ASD children in regular classrooms have increased social
interaction, a larger social network and have more advanced individualized
education plan goals later in their academic careers (Fryxell and Kennedy,
1995). Whether a child is fully or partially included in a regular classroom or
placed in a self-contained setting, each ASD child will need to have an indi-vidualized
plan of care that carefully and specifically articulates goals and the
techniques to be used to reach those goals. In addi-tion, specific measures of
goal attainment and regular review of the plan should be a part of this
important intervention. In order to establish these goals and plans, a full
assessment of the child’s strengths and weaknesses must be completed through
the efforts of numerous skilled professionals. Educational plans must
incor-porate academic, social and behavioral goals.
Pharmacotherapy
At this time, there are no pharmacological agents
with US Food and Drug Administration (FDA)-approved labeling specific for the
treatment of ASD in either children or adults. Many of the symptoms commonly
seen in ASD (rituals, aggressive behavior and hyperactivity) are also commonly
seen in children, adoles-cents and adults with mental retardation but without a
PDD. Some of the pharmacological strategies for the treatment of autistic
dis-order have been extrapolated from studies of related conditions, largely in
adults, but including attention-deficit/hyperactivity disorder and OCD.
Clinicians and families should be reminded before any treatment is initiated
that:
• Current treatments target symptoms.
• Current treatments do not target a specifi c
etiological mechanism for ASD.
• Anecdotal reports do not establish effi cacy,
effectiveness, or safety for any treatment.
• Controlled, double-blind trials (preferably with
replication) are the contemporary standard for determining if a treatment is
safe and appropriate.
• All treatments have side effects.
Before specific pharmacological agents are
discussed, it must be stressed that one should not use psychopharmacological
agents with the expectation that they will cure children with autistic disor-der
as many parents and teachers of children with autistic disorder expect
medication to eliminate core social, cognitive and commu-nication dysfunction.
There is no pharmacological substitute for appropriate educational, behavioral,
psychotherapeutic, vocational and recreational programming. It is essential to
remember and to remind parents, teachers and others that medication should
always be seen as an adjunct to these core interventions that address the
developmental challenges associated with these disorders.
Because many individuals with ASD have impairments
in language and social communication, the use of rating scales be-comes an
essential part of the treatment. Standard rating scales provide the
pharmacotherapist with a framework in which to assess response to medication
and a relatively straightforward way to collect standard information about the
patient’s function-ing in a variety of settings. The Aberrant Behavior
Checklist – Community Version (Aman, 1994) covers many target symptom areas for
most patients with ASD. Although rating scales cannot replace careful clinical
examination of the patient and interviews with parents and teachers, they may
be graphed next to dosages of medications to assist in treatment planning in
response to the patient’s clinical condition. This is often not only helpful in
mak-ing clinical decisions but also gives families and service provid-ers a
concrete sense of how a treatment is progressing.
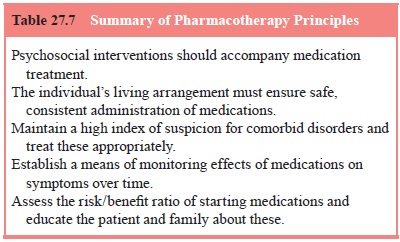
The use of medications to treat autistic disorder
and other ASDs appears to have significant potential as an adjunct to
edu-cational, environmental and social interventions. It is a reason-able goal
for the pharmacotherapist to adopt the judicious use of psychopharmacological
agents to assist in alleviating symptoms that have been found to respond to
pharmacological intervention (Table 27.7). This focus on facilitating
adaptation requires atten-tion to five important principles:
·
Environmental manipulations, including behavioral
treat-ment, may be as effective as, if not more effective than, medi-cation for
selected symptomatic treatment.
·
It is essential that the living arrangement for the
individual must ensure safe and consistent administration and monitor-ing of
the medication to be used.
·
Individuals with autistic disorder and other ASDs
often have other DSM-IV-TR Axis I disorders. If a comorbid DSM-IV-TR Axis I
disorder is present, standard treatment for that disorder should be initiated
first.
· Medication should be selected on the basis of potential effects on target symptoms and there should be an established way of specifically monitoring the response to the treatment over time.
· A careful
assessment of the risk/benefit ratio must be made before initiating treatment
and, to the extent possible, the pa-tient’s caretakers and the patient must
understand the risks and benefits of the treatment.
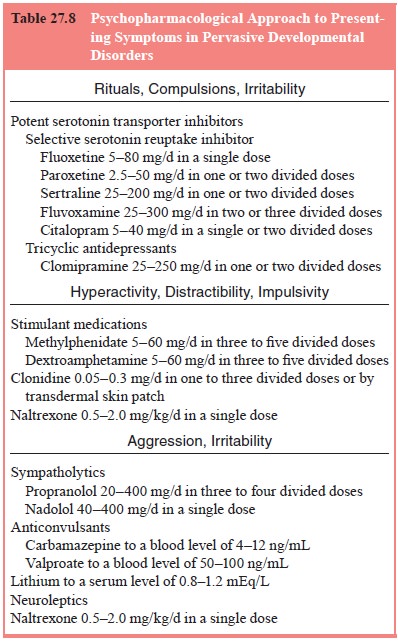
Potent Serotonin Transporter Inhibitors
This class of agents includes selective serotonin
reuptake inhibi-tors (SSRIs) as well as the less selective but potent clomipramine,
a tricyclic antidepressant (Table 27.8). This group of medications is most
effective when insistence on routines or rituals are present to the point of
manifest anxiety or aggression in response to interrup-tion of the routines or
rituals, or after the onset of another disorder such as major depressive
disorder or OCD. The common side effects associated with SSRIs are motor
restlessness, insomnia, elation, ir-ritability and decreased appetite. Because
many of these symptoms may be present in the often cyclical natural course of
ASD before the medication is initiated, the emergence of new symptoms, a
dif-ferent quality of the symptoms, and occurrence of these symptoms in a new
cluster are clues that the symptoms are side effects of medi-cation rather than
part of the natural course of the disorder.
Stimulants
Small but significant reductions in inattention and hyperactivity ratings may be seen in children with autistic disorder in response to stimulants such as methylphenidate and dextroamphetamine
In a placebo-controlled crossover study, eight of
13 subjects showed a reduction of at least 50% on methylphenidate (Handen et al., 2000). However, stereotypies may
worsen, so drug trials for the
individual patient must always be assessed to determine whether the therapeutic
effects outweigh side effects. A key dis-tinction in assessing attentional
problems of children with ASD is the distinction between poor sustained
attention (characteris-tic of children with attention-deficit/hyperactivity
disorder) and poor joint attention (characteristic of children with autistic
disor-der). Problems in joint attention require educational and behavio-ral
interventions or treatment of rituals with an SSRI. Problems in maintenance of
attention of the type seen in attention-deficit/ hyperactivity disorder are
more likely to respond to stimulants.
Sympatholytics
The alpha-2-adrenergic receptor agonist
clonidine reduced irri-tability as well as hyperactivity and impulsivity in two
double-blind, placebo-controlled trials. However, tolerance developed several
months after initiation of the treatment in each child who was treated long
term but may have been reduced in several cases by administering clonidine in
the morning and then 6 to 8 hours later with a 16- to 18-hour interval between
the last dose of one day and the first dose of the next day. If tolerance does
develop, the dose should not be increased because tolerance to sedation does
not occur, and sedation may lead to increased ag-gression due to disinhibition
or decreased cognitive control of impulses. Adrenergic receptor antagonists,
such as propranolol and naldolol, have not been tested in double-blind trials
in ASD. However, open trials have reported the use of these medications in the treatment
of aggression and impulsivity in developmental disorders including autistic
disorder.
Neuroleptics
Typical Neuroleptics
Because they were among the first modern
psychopharmaco-logical agents, typical neuroleptics have been among the most
extensively studied drugs in autistic disorder. Trifluoperazine, thioridazine,
haloperidol and pimozide have been studied in dou-ble-blind, controlled trials
lasting from 2 to 6 months. Reduction of fidgetiness, interpersonal withdrawal,
speech deviance and stereotypes has been documented in response to these.
How-ever, patients with autistic disorder are as vulnerable to poten-tially
irreversible tardive dyskinesia as any other group of young patients. Owing to
the often earlier age at initiation of pharma-cotherapy, patients with ASD
treated with typical neuroleptics may be at higher risk because of the
potential increased lifetime exposure of medication limiting their routine use
in the care of patients with ASD, especially as first-line treatments.
Atypical Neuroleptics
Because of the positive response of many children
with autis-tic disorder to typical neuroleptics, similar medications with
re-duced risk of tardive dyskinesia must be considered. In addition, atypical
neuroleptics are often effective in treating the negative symptoms of
schizophrenia, which seem similar to several of the social deficits in autistic
disorder. Both risperidone and olanzap-ine have shown promise in open label
trials in reducing hyperac-tivity, impulsivity, aggressiveness and obsessive
preoccupations.
A double-blind, placebo-controlled study found
risperidone to be more effective than placebo in the treatment of repetitive
behav-ior, aggression and irritability (McDougle et al., 1998).
Anticonvulsants
Because 25 to 33% of patients with autistic
disorder have seizures, the psychopharmacological management of patients with
autistic disorder or other ASD must take into consideration the past or current
history of epilepsy and the potential role of anticonvulsants. In an open trial
of divalproex, 10 of 14 patients responded favorably, showing improvements in
affective stability, impulsivity and aggression (Hollander et al., 2001). Because barbiturates have been associated with
hyperactivity, depression and cognitive impairment, they should be changed to
an alternative drug, depending on the seizure and avoided when possible. In
addition, phenytoin (Dilantin) is sedating and can cause hypertrophy of the
gums and hirsutism, which may contribute to the social challenges for people
with autistic disorder. Carbamazepine and valproate may have positive
psychotropic effects, particularly when cyclical irritability, insomnia and
hyperactivity are present.
Naltrexone
Double-blind trials have demonstrated that
naltrexone, an opiate antagonist, has little efficacy in treating the core
social and cognitive symptoms of autistic. While the use of naltrexone as a
specific treatment for autistic disorder no longer seems to be likely, it may
have a role in the treatment of self-injurious behavior, although the
controlled data are equivocal. Controlled trials have shown a modest reduction
in symptoms of hyperactivity and restlessness sometimes associated with
autistic disorder. Potential side effects include nausea and vomiting.
Naltrexone may have an adverse effect on the outcome of Rett’s disorder on the
basis of a relatively large, randomized, double-blind, placebo-controlled trial
(Percy et al., 1994).
Lithium
Adolescents and adults with autistic disorder often
exhibit symp-toms in a cyclic manner and so there is much interest in how these
patients might respond to agents typically used in bipolar disorder. A single
open trial of lithium revealed no significant im-provement in symptoms in
patients with autistic disorder without bipolar disorder (Campbell et al., 1972).
Anxiolytics
Benzodiazepines have not been studied
systematically in chil-dren and adolescents with autistic disorder. However,
their use to reduce anxiety in short-term treatment, such as before dental
procedures, is similar to their use in management of anxiety in people without
a PDD. One open label study has found a decrease in anxiety and irritability in
patients receiving the anxiolytic bus-pirone (Buitelaar et al., 1998).
Glutamatergic Antagonists
Interest in these agents has been sparked by the
hypothesis that ASDs may be a disorder of hypoglutaminergic activity. In a
dou-ble-blind, placebo-controlled study of the glutamatergic antago-nist
amantadine hydrochloride, there were substantial improve-ments in
clinician-rated hyperactivity and irritability, although parental reports did
not reach statistical significance (King et
al., 2001).
Other Treatments
Pyridoxine,
the water-soluble essential vitamin B6, has been used extensively as
a pharmacological treatment in autistic disorder. In the doses used for autistic
disorder, it is not being used as a cofactor for normally regulated enzyme
function or as a vita-min; rather, it is used to modulate the function of
neurotrans-mitter enzymes, such as tryptophan hydroxylase and tyrosine
hydroxylase. Recent reviews have concluded that there are little data to
support the claim that vitamin B6 improves developmental course. The
same is true for using fenfluramine, naloxone and secretin.
Related Topics