Chapter: Essentials of Psychiatry: Childhood Disorders: The Autism Spectrum Disorders
Autism Spectrum Disorders: Assessment and Differential Diagnosis
Assessment and Differential
Diagnosis
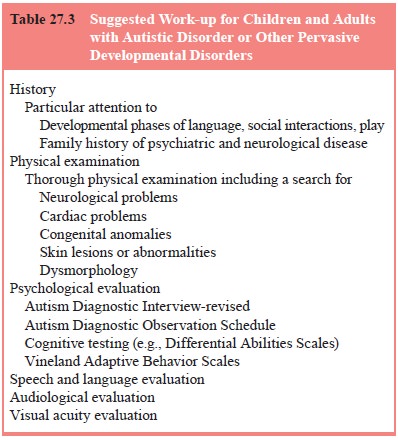
The diagnosis of ASD first involves completing a
comprehen-sive psychiatric examination (Table 27.3). The clinician should
obtain a full developmental history, including all information regarding
pregnancy and delivery. While questioning about neonatal development,
particular attention should be paid tosocial, communicative and motor
milestones. The clinician needs to understand fully the child’s adaptive
skills, includ-ing which tasks can be undertaken independently, including
grooming skills, feeding skills and the ability to self-initiate. There should
be a sense of the child’s vocabulary, receptive and expressive language skills,
articulation and pragmatic commu-nication. A full medical history should be
obtained, and should include queries regarding any hearing or vision problems, any
history of seizures and information regarding the use of any medications.
Because these children dislike novelty, the first
visit to the clinician’s office is sometimes an anxiety-provoking undertak-ing.
It is not unusual (and is in fact helpful diagnostically) to al-low a child
with ASD to extensively explore the clinician’s office, looking under desks or
opening drawers, in an attempt to become familiar with the surroundings. Some
children will appear shy and self-absorbed. It is ideal if the clinician can
arrange an op-portunity to see the child in another environment in addition to
the office. Observation of the child interacting with the parents and siblings
is helpful in understanding modes of interaction and social skills. If the
child is having difficulty, it is usually prefer-able, especially on the first
visit, to allow the parents to inter-vene. This will allow the clinician to see
how (effectively) the family responds to this distress, and how the child
responds to the efforts of caregivers to soothe the child. During observation,
the clinician needs to assess social interaction, communication, unusual
behaviors and all other information in the context of de-velopmental level.
A full physical examination should be undertaken
includ-ing observations for dysmorphic features and unusual dermato-logic
lesions. The clinician must maintain a high suspicion for seizures in this
population, both when taking the history and dur-ing the examination. A full
neurological examination should be made with an emphasis on motor impairments.
A Wood’s light examination for hypopigmented lesions consistent with tuberous
sclerosis should be made
There are no diagnostic laboratory tests for ASD.
If the child has not had routine tests (blood count, liver function tests,
thyroid, lead level, etc.), these should be completed, as with any child.
Patients with mental retardation or dysmorphology should have chromosomal
analysis performed. Fragile X testing and fluorescent in situ hybridization
(FISH) studies for possible in-terstitial duplication of 15q11–13 should be
suggested after con-sultation with the family. There should be a low threshold
for ordering an electroencephalogram (EEG), and one should always be ordered in
the context of unusual movements, regressive be-havior, regressive loss of
previously acquired sleep, or in the face of unusually poor sleep. Structural
brain imaging (i.e., MRI) should take place only if the physical examination or
history sug-gests that a treatable lesion is present. Carried out routinely,
these scans have a very low clinical yield, are quite expensive, and in this
population often require anesthesia, a seemingly unneces-sary risk.
Consultative services should be utilized as needed with pediatric neurologists
and geneticists. Difficulties with motor de-velopment will often mean a
referral to an occupational and/or physical therapist. Children with Rett’s
syndrome will often re-quire referral to neurologists and developmental
pediatricians.
All children with autism require a careful language
assess-ment that may include hearing testing and assessment of expres-sive and
receptive, verbal and nonverbal language. Speech and language therapists
trained to work with this population are an essential part of the assessment
team.
Children with ASD should have a neuropsychological
as-sessment at the time of initial assessment and at periodic intervals
thereafter. The initial evaluation helps establish the diagnosis and a baseline
level of functioning. Additionally, it can be utilized to make the appropriate
adjustments in the child’s educational plan. The later evaluations serve to
chart progress, evaluate the success of (pharmacological, behavioral and
academic) interven-tions, and to assess for possible regression in particular
areas.
While there are many rating scales and structured
interviews to assist in making the diagnosis of ASD, the current gold standard
in diagnostic assessment is the autism diagnostic observation schedule-generic
(ADOS-G) (Lord et al., 2000). This is
often given with the autism diagnostic inventory-revised (ADI-R) (Lord et al., 1994), which is a comprehensive,
clinician-administered interview of the patient’s primary caregiver and covers
most developmental and behavioral aspects of autism. The ADI/ADOS combination
is now established as a reliable and valid method for making the diagnosis of
ASD.
Related Topics