Chapter: Obstetrics and Gynecology: Embryology and Anatomy
Anatomy of Uterus and Pelvic Support
Uterus and Pelvic Support
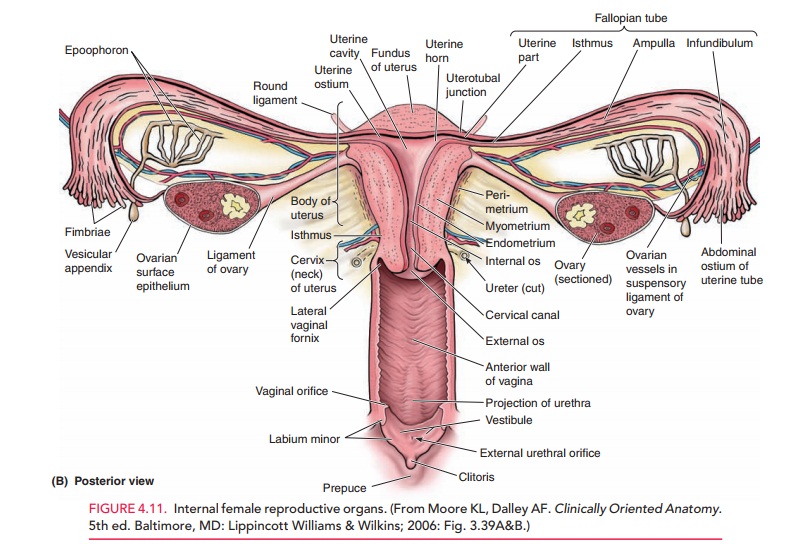
The uterus lies between the rectum
and the bladder (Fig. 4.11). Various
pelvic ligaments help support the uterus and other pelvic organs. The broad ligament overlies the structures
and connective tissue immediately adjacent to the uterus. Because it contains
the uterine arteries and veins and the ureters, it is important to identify the
broad ligament during surgery. The infundibulopelvic
lig-ament connects the ovary to the posterior abdominal wall and is
composed mainly of the ovarian vessels. The uterosacral ligament connects the uterus at the level of thecervix
to the sacrum and is therefore its primary support. The cardinal ligament is attached to the side of the uterus immediately
inferior to the uterine artery. The sacro-spinous ligament connects the
sacrum to the iliac spine andis not attached to the uterus. This ligament is
frequently used surgically to support the pelvic viscera.
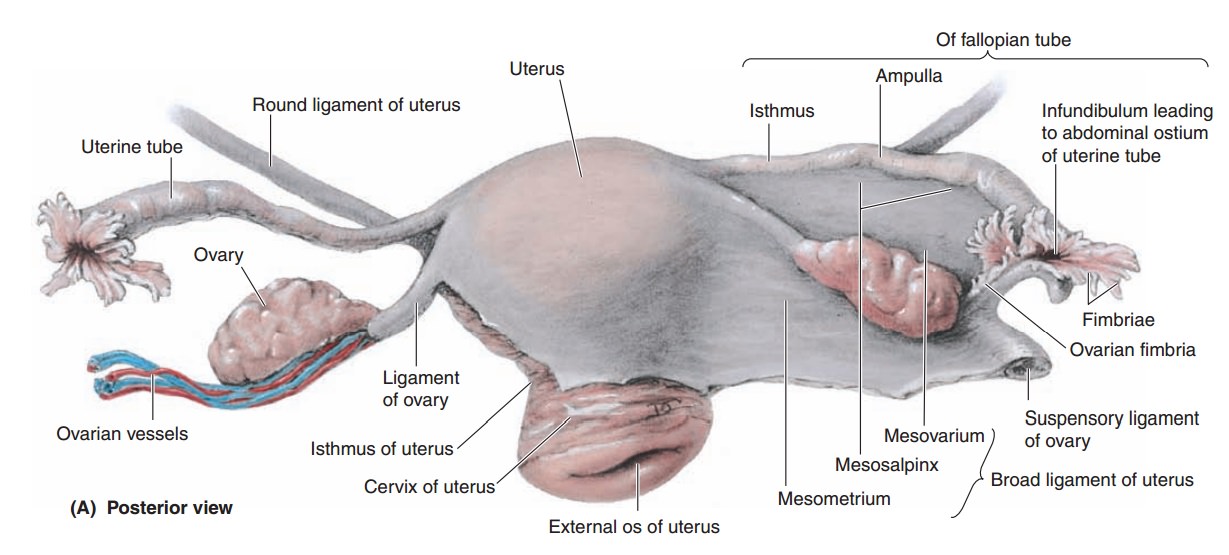
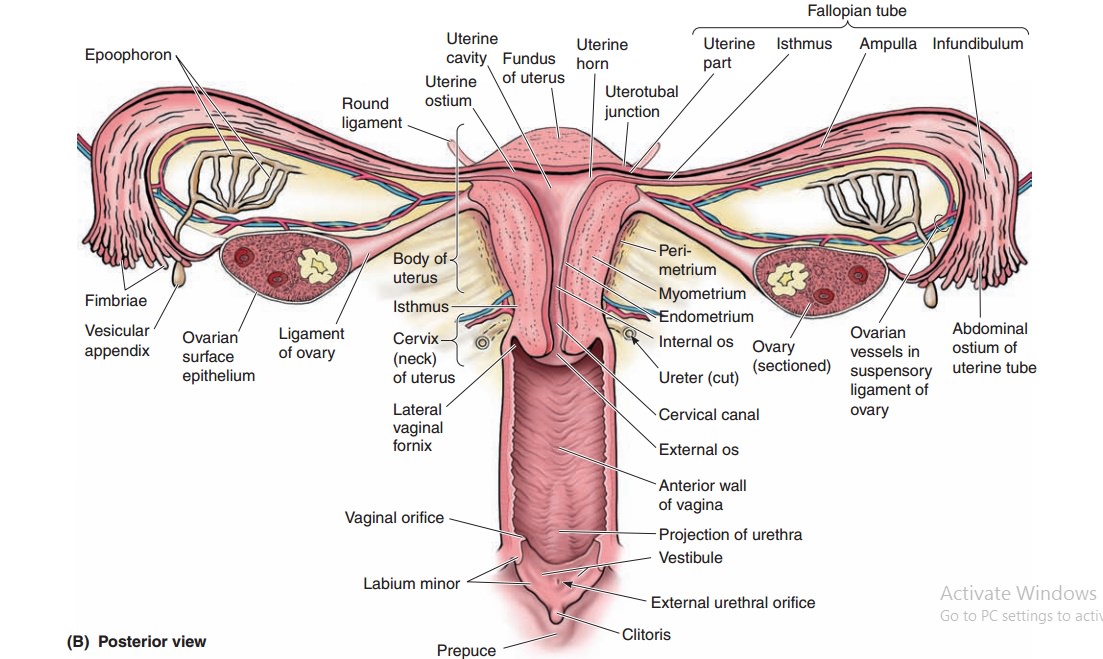
The two major portions of the
uterus are the cervix and the body
(corpus), which are separated by a narrower isthmus. The length of the
cervix is established at puberty. Before puberty, the relative lengths of the
body of the uterus and cervix are approximately equal; after puberty, under the
influence of increased estrogen levels, the ratio of the body to the cervix
changes to between 2:1 and 3:1. The part of the body where the two uterine
tubes enter it is called the cornu.
The part of the corpus above the cornu is referred to as the fundus. In a woman
who has had no children, the uterus is approximately 7 to 8 cm long and 4 to 5
cm wide at the widest part. The cervix is relatively cylindrical in shape and
is 2 to 3 cm long. The body is gen-erally pear-shaped, with the anterior
surface flat and the posterior surface convex. In cross section, the lumen of
the uterine body is triangular.
The wall of the uterus consists
of three layers:
1. The inner
mucosa, or endometrium, consists of
sim-ple columnar epithelium with underlying connective tissue, which changes in
structure during the men-strual cycle.
2.
The middle layer, or myometrium, consists of smooth muscle.
This layer becomes greatly distensible during pregnancy; during labor, the
smooth muscle in this layer contracts in response to hormonal stimulation
3. The
outermost layer, or perimetrium,
consists of a thin layer of connective tissue. It is distinct from the para-metrium, a subserous extension of
the uterus betweenthe layers of the broad ligament.
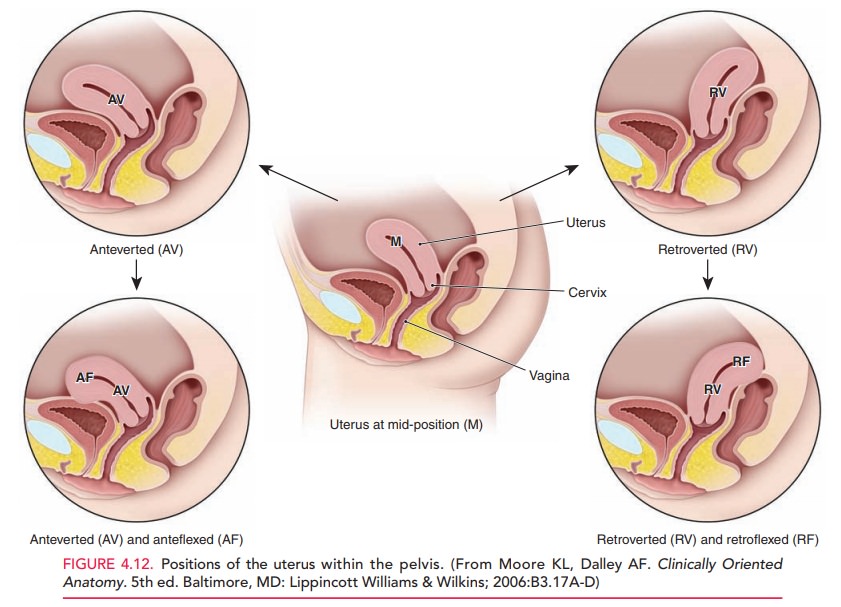
The position of the uterus can
vary depending on the rela-tionship of a straight axis that extends from the
cervix to the uterine fundus to the horizontal. When a woman is in the dorsal
lithotomy position, the uterus may be bent forward (anteversion, AV), slightly forward but functionally straight (mid-position, MP), or bent backward (retroversion, RV). The top of the uterus
can also fold forward (anteflexion,AF)
or backward (retroflexion, RF). Five
combinationsof these configurations are possible (Fig. 4.12). The posi-tion of
the uterus is clinically important. For example, estimation of gestational age
in the late part of the first trimester may be difficult when the uterus is in
the RVRF or RV positions. Risk of uterine perforation during pro-cedures such
as dilatation & curettage or insertion of an intrauterine device is
increased in a woman with a retro-flexed or anteflexed uterus. Applying
traction on the cervix to pull the uterine canal into a straight line can
greatly reduce this risk.
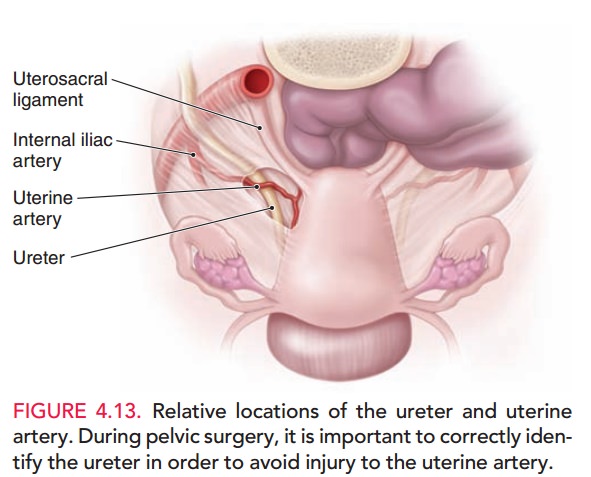
The blood supply to the uterus
comes primarily from the uterine arteries, with a contribution from the ovarian
arteries, whereas the venous plexus drains through the uterine vein.
Of
particular importance in pelvic surgery is the relative position of the uterine
artery to the ureter.
The arteries travel in a lateral
to medial direction at the level of the internal os of the cervix. At the point
where they meet the uterus, they overlie the ureter. This proximity can cause
inadvertent injury during pelvic surgery. The ureters lie between 1.5 cm and 3
cm from the uterine side-wall at this point (Fig. 4.13).
Related Topics