Chapter: Medical Surgical Nursing: Assessment and Management of Patients With Biliary Disorders
Anatomy and Function of the Gallbladder
ANATOMY OF THE GALLBLADDER
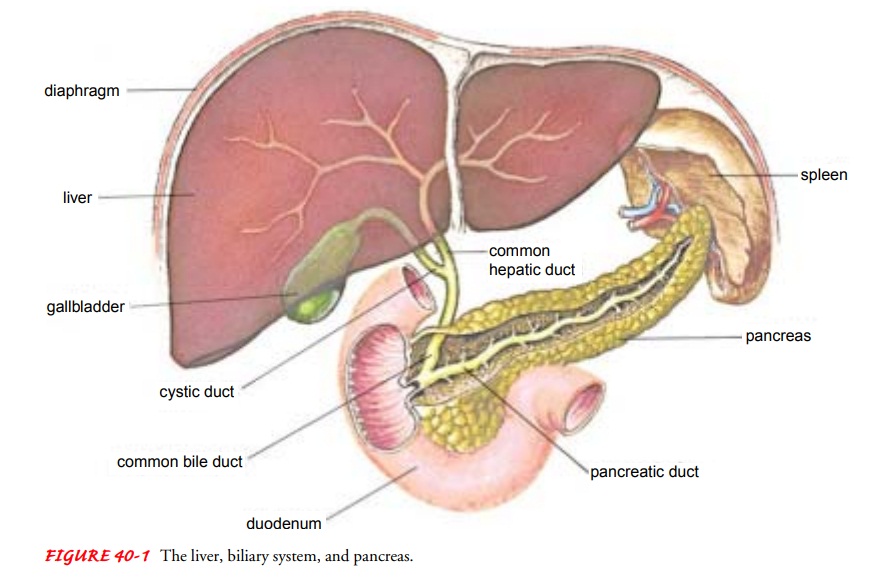
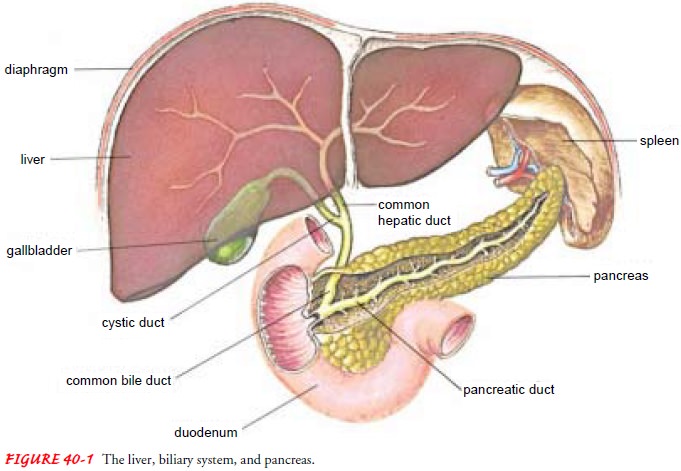
The
gallbladder, a pear-shaped, hollow, saclike organ, 7.5 to 10 cm (3 to 4 in)
long, lies in a shallow depression on the inferior sur-face of the liver, to
which it is attached by loose connective tissue. The capacity of the gallbladder
is 30 to 50 mL of bile. Its wall is composed largely of smooth muscle. The
gallbladder is connected to the common bile duct by the cystic duct (Fig.
40-1).
FUNCTION OF THE GALLBLADDER
The
gallbladder functions as a storage depot for bile. Between meals, when the
sphincter of Oddi is closed, bile produced by the hepatocytes enters the
gallbladder. During storage, a large portion of the water in bile is absorbed
through the walls of the gall-bladder, so that gallbladder bile is five to ten
times more concen-trated than that originally secreted by the liver. When food
enters the duodenum, the gallbladder contracts and the sphincter of Oddi
(located at the junction where the common bile duct en-ters the duodenum)
relaxes. Relaxation of the sphincter of Oddi allows the bile to enter the
intestine. This response is mediated by secretion of the hormone cholecystokinin–pancreozymin(CCK-PZ) from
the intestinal wall. Bile is composed of waterand electrolytes (sodium,
potassium, calcium, chloride, and bi-carbonate) and significant amounts of
lecithin, fatty acids, cho-lesterol, bilirubin, and bile salts. The bile salts,
together with cholesterol, assist in emulsification of fats in the distal
ileum. They then are reabsorbed into the portal blood for return to the liver
and again excreted into the bile. This pathway from hepatocytes to bile to
intestine and back to the hepatocytes is called the enterohepatic circulation.
Because of the enterohepatic cir-culation, only a small fraction of the bile
salts that enter the in-testine are excreted in the feces. This decreases the
need for active synthesis of bile salts by the liver cells.
If the
flow of bile is impeded (ie, with gallstones in the bile ducts), bilirubin, a
pigment derived from the breakdown of red blood cells, does not enter the
intestine. As a result, bilirubin levels in the blood increase. This results,
in turn, in increased renal excretion of urobilinogen, which results from
conversion of bilirubin in the small intestine, and decreased excretion in the
stool. These changes produce many of the signs and symptoms seen in gallbladder
disorders.
Related Topics