Chapter: Medical Surgical Nursing: Assessment and Management of Patients With Biliary Disorders
Tumors of the Head of the Pancreas
TUMORS
OF THE HEAD OF THE PANCREAS
Sixty
to eighty percent of pancreatic tumors occur in the head of the pancreas.
Tumors in this region of the pancreas obstruct the common bile duct where the
duct passes through the head of the pancreas to join the pancreatic duct and
empty at the ampulla of Vater into the duodenum. The tumors producing the
obstruction may arise from the pancreas, the common bile duct, or the am-pulla
of Vater.
Clinical Manifestations
The
obstructed flow of bile produces jaundice, clay-colored stools, and dark urine.
Malabsorption of nutrients and fat-soluble vitamins may result from obstruction
by the tumor to entry of bile in the gastrointestinal tract. Abdominal
discomfort or painand pruritus may be noted, along with anorexia, weight loss,
and malaise. If these signs and symptoms are present, cancer of the head of the
pancreas is suspected.
The
jaundice of this disease must be differentiated from that due to a biliary
obstruction caused by a gallstone in the common duct, which is usually
intermittent and appears typically in obese patients, most often women, who
have had previous symptoms of gallbladder disease.
Assessment and Diagnostic Findings
Diagnostic
studies may include duodenography, angiography by hepatic or celiac artery
catheterization, pancreatic scanning, per-cutaneous transhepatic
cholangiography, ERCP, and percutaneous needle biopsy of the pancreas. Results
of a biopsy of the pancreas may aid in the diagnosis.
Medical Management
Before
extensive surgery can be performed, a fairly long period of preparation is
often necessary because the patient’s nutritional and physical condition is
often quite compromised. Various liver and pancreatic function studies are
performed. A diet high in pro-tein along with pancreatic enzymes is often
prescribed. Preoper-ative preparation includes adequate hydration, correction
of prothrombin deficiency with vitamin K, and treatment of anemia to minimize
postoperative complications. Parenteral nutrition and blood component therapy
are frequently required.
A
biliary-enteric shunt may be performed to relieve the jaun-dice and, perhaps,
to provide time for a thorough diagnostic eval-uation. Total pancreatectomy
(removal of the pancreas) may be performed if there is no evidence of direct
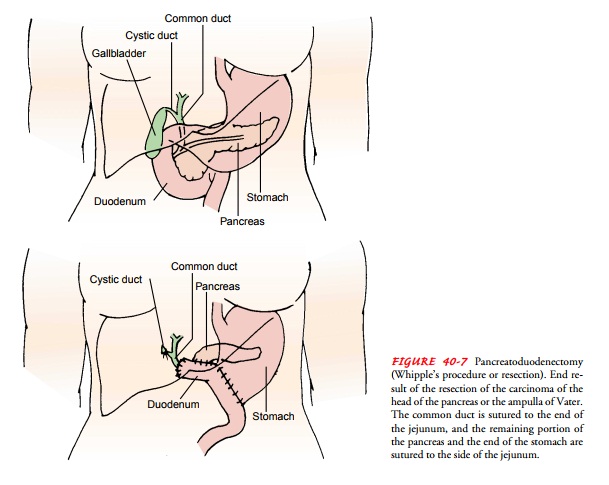
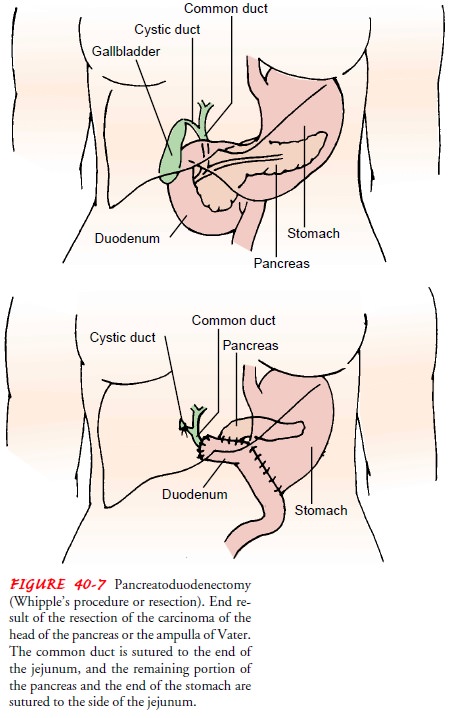
extension of the tumor to adjacent tissues or regional lymph nodes. A
pancreaticoduo-denectomy (Whipple’s procedure or resection) is used for
poten-tially resectable cancer of the head of the pancreas (Fig. 40-7). This
procedure involves removal of the gallbladder, distal portion of the stomach,
duodenum, head of the pancreas, and common bile duct and anastomosis of the
remaining pancreas and stomach to the je-junum (Stanford, 2001). The result is
removal of the tumor, al-lowing flow of bile into the jejunum. When the tumor
cannot be excised, the jaundice may be relieved by diverting the bile flow into
the jejunum by anastomosing the jejunum to the gallbladder, a procedure known
as cholecystojejunostomy.
The
postoperative management of patients who have under-gone a pancreatectomy or a
pancreaticoduodenectomy is simi-lar to the management of patients after
extensive gastrointestinal and biliary surgery. The patient’s physical status
is often less than optimal, increasing the risk for postoperative
complications. Hemorrhage, vascular collapse, and hepatorenal failure remain
the major complications of these extensive surgical procedures. The mortality
rate after these procedures has improved because of advances in nutritional
support and improved surgical tech-niques. A nasogastric tube and suction and
parenteral nutrition allow the gastrointestinal tract to rest while promoting
adequate nutrition.
Nursing Management
Preoperatively and postoperatively, nursing care is directed to-ward promoting patient comfort, preventing complications, and assisting the patient to return to and maintain as normal and comfortable a life as possible. The nurse closely monitors the pa-tient in the intensive care unit after surgery; the patient will have multiple
intravenous and arterial lines in place for fluid and blood replacement as well
as for monitoring arterial pressures, and is on a mechanical ventilator in the
immediate postoperative period. It is important to give careful attention to
changes in vital signs, arterial blood gases and pressures, pulse oximetry,
laboratory val-ues, and urine output. The nurse must also consider the
patient’s compromised nutritional status and risk for bleeding. Depend-ing on
the type of surgical procedure performed, malabsorption syndrome and diabetes
mellitus are likely; the nurse must address these issues during acute and
long-term patient care.
Although
the patient’s physiologic status is the focus of the health care team in the
immediate postoperative period, the pa-tient’s psychological and emotional
state must be considered, along with that of the family. The patient has
undergone major and risky surgery and is critically ill; thus, anxiety and
depression may affect recovery. The immediate and long-term outcome of this
extensive surgical resection is uncertain, and the patient and family require
emotional support and understanding in the crit-ical and stressful preoperative
and postoperative periods.
PROMOTING HOME AND COMMUNITY-BASED CARE
Teaching Patients Self-Care.
The patient
who has undergone thisextensive surgery requires careful and thorough
preparation for self-care at home. The nurse instructs the patient and family
about the need for modifications in the diet because of malabsorption and
hyperglycemia resulting from the surgery. It is important to instruct them
about the continuing need for pancreatic enzyme replacement, a low-fat diet,
and vitamin supplementation.
The
nurse teaches the patient and family strategies to relieve pain and discomfort,
along with strategies to manage drains, if present, and to care for the
surgical incision. The patient and family members may require instruction about
use of patient-controlled analgesia, parenteral nutrition, wound care, skin
care, and management of drainage. It is important to describe, verbally and in
writing, the signs and symptoms of complications, and to teach the patient and
family about indicators of complications that should be reported promptly.
Discharge
of the patient to a long-term care setting may be warranted after surgery as
extensive as pancreatectomy or pan-creaticoduodenectomy, particularly if the
patient’s preopera-tive status was not optimal. Efforts are made to communicate
to the long-term care staff about the teaching that has been pro-vided so that
instructions can be clarified and reinforced. Dur-ing the recovery or long-term
phase of care, the patient and family receive further instructions about care
that they will carry out at home.
Continuing Care.
A referral
for home care may be indicated whenthe patient returns home. The home care
nurse assesses the pa-tient’s physical and psychological status and the ability
of the pa-tient and family to manage needed care. The home care nurse provides
needed physical care and monitors the adequacy of pain management. In addition,
it is important to assess the patient’s nutritional status and monitor the use
of parenteral nutrition. The nurse discusses the use of hospice services with
the patient and family and makes a referral if indicated.
Related Topics