Chapter: Medical Surgical Nursing: Assessment and Management of Patients With Biliary Disorders
The Pancreas
THE
PANCREAS
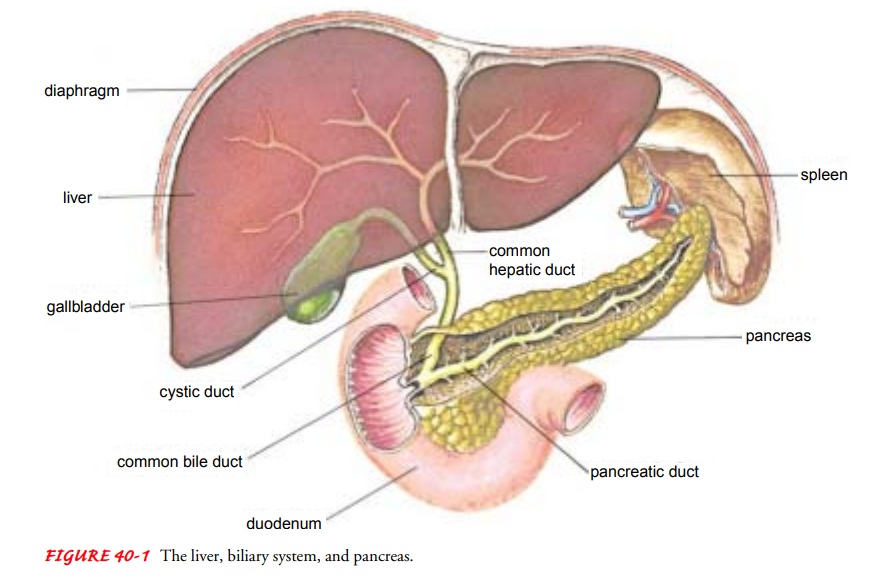
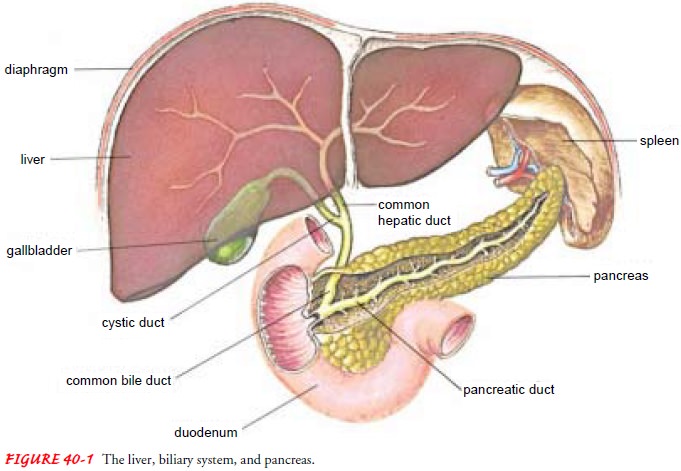
The
pancreas, located in the upper abdomen, has endocrine as well as exocrine
functions (see Fig. 40-1). The secretion of pan-creatic enzymes into the gastrointestinal
tract through the pan-creatic duct represents its exocrine function. The
secretion of insulin, glucagon, and somatostatin directly into the bloodstream
represents its endocrine function.
Exocrine Pancreas
The
secretions of the exocrine portion of the pancreas are col-lected in the
pancreatic duct, which joins the common bile duct and enters the duodenum at
the ampulla of Vater. Surrounding the ampulla is the sphincter of Oddi, which
partially controls the rate at which secretions from the pancreas and the
gallbladder enter the duodenum.
The secretions of the exocrine pancreas are digestive enzymes high in protein content and an electrolyte-rich fluid. The secre-tions are very alkaline because of their high concentration of sodium bicarbonate and are capable of neutralizing the highly acid gastric juice that enters the duodenum. The enzyme secre-tions include amylase, which aids in the digestion of carbohy-drates; trypsin, which aids in the digestion of proteins; and lipase, which aids in the digestion of fats. Other enzymes thatpromote the breakdown of more complex foodstuffs are also secreted.
Hormones
originating in the gastrointestinal tract stimulate the secretion of these
exocrine pancreatic juices. Secretin
is the major stimulus for increased bicarbonate secretion from the pan-creas,
and the major stimulus for digestive enzyme secretion is the hormone CCK-PZ.
The vagus nerve also influences exocrine pancreatic secretion.
Endocrine Pancreas
The
islets of Langerhans, the endocrine part of the pancreas, are col-lections of
cells embedded in the pancreatic tissue. They are com-posed of alpha, beta, and
delta cells. The hormone produced by the beta cells is called insulin; the
alpha cells secrete glucagon and the delta cells secrete somatostatin.
INSULIN
A
major action of insulin is to lower blood glucose by permitting entry of the
glucose into the cells of the liver, muscle, and other tissues, where it is
either stored as glycogen or used for energy. In-sulin also promotes the
storage of fat in adipose tissue and the synthesis of proteins in various body
tissues. In the absence of in-sulin, glucose cannot enter the cells and is
excreted in the urine. This condition, called diabetes mellitus, can be
diagnosed by high levels of glucose in the blood. In diabetes mellitus, stored
fats and protein are used for energy instead of glucose, with consequent loss
of body mass. The level of glucose in the blood normally regulates the rate of
insulin secretion from the pancreas.
GLUCAGON
The
effect of glucagon (opposite to that of insulin) is chiefly to raise the blood
glucose by converting glycogen to glucose in the liver. Glucagon is secreted by
the pancreas in response to a de-crease in the level of blood glucose.
SOMATOSTATIN
Somatostatin
exerts a hypoglycemic effect by interfering with re-lease of growth hormone
from the pituitary and glucagon from the pancreas, both of which tend to raise
blood glucose levels.
Endocrine Control of Carbohydrate Metabolism
Glucose
for body energy needs is derived by metabolism of in-gested carbohydrates and
also from proteins by the process of glu-coneogenesis. Glucose can be stored
temporarily in the liver, muscles, and other tissues in the form of glycogen.
The endocrine system controls the level of blood glucose by regulating the rate
at which glucose is synthesized, stored, and moved to and from the bloodstream.
Through the action of hormones, blood glucose is normally maintained at about
100 mg/dL (5.5 mmol/L). Insulin is the primary hormone that lowers the blood
glucose level. Hor-mones that raise the blood glucose level are glucagon,
epinephrine, adrenocorticosteroids, growth hormone, and thyroid hormone.
The
endocrine and exocrine functions of the pancreas are in-terrelated. The major
exocrine function is to facilitate digestion through secretion of enzymes into
the proximal duodenum. Se-cretin and CCK-PZ are hormones from the
gastrointestinal tract that aid in the digestion of food substances by
controlling the se-cretions of the pancreas. Neural factors also influence
pancreatic enzyme secretion. Considerable dysfunction of the pancreas must
occur before enzyme secretion decreases and protein and fat di-gestion becomes
impaired. Pancreatic enzyme secretion is nor-mally 1,500 to 2,500 mL/day.
Gerontologic Considerations
There
is little change in the size of the pancreas with age. There is, however, an
increase in fibrous material and some fatty depo-sition in the normal pancreas
in patients older than 70 years of age. Some localized arteriosclerotic changes
occur with age. There is also a decreased rate of pancreatic secretion
(decreased lipase, amylase, and trypsin) and bicarbonate output in older
patients. Some impairment of normal fat absorption occurs with increas-ing age,
possibly because of delayed gastric emptying and pan-creatic insufficiency.
Decreased calcium absorption may also occur. These changes require care in
interpreting diagnostic tests in the normal elderly person and in providing
dietary counseling.
Related Topics