Chapter: Medical Surgical Nursing: Assessment and Management of Patients With Biliary Disorders
Cholelithiasis - Disorders of the Gallbladder
CHOLELITHIASIS
Calculi,
or gallstones, usually form in the gallbladder from the solid constituents of
bile; they vary greatly in size, shape, and com-position (Fig. 40-2). They are
uncommon in children and young adults but become increasingly prevalent after
40 years of age. The incidence of cholelithiasis increases thereafter to such
an ex-tent that up to 50% of those over the age of 70 and over 50% of those
over 80 will develop stones in the bile tract (Borzellino, deManzoni &
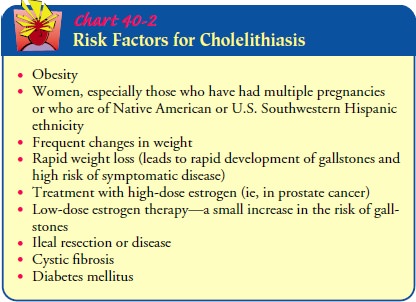
Ricci, 1999). Chart 40-2 identifies common risk factors.
Pathophysiology
There
are two major types of gallstones: those composed pre-dominantly of pigment and
those composed primarily of choles-terol. Pigment stones probably form when
unconjugated pigments in the bile precipitate to form stones; these stones
account for about one third of cases in the United States (Donovan, 1999). The
risk of developing such stones is increased in patients with cirrhosis,
hemolysis, and infections of the biliary tract. Pigment stones cannot be
dissolved and must be removed surgically.
Cholesterol
stones account for most of the remaining cases of gallbladder disease in the
United States. Cholesterol, a normal constituent of bile, is insoluble in
water. Its solubility depends on bile acids and lecithin (phospholipids) in
bile. In gallstone-prone patients, there is decreased bile acid synthesis and
increased cho-lesterol synthesis in the liver, resulting in bile supersaturated
with cholesterol, which precipitates out of the bile to form stones. The
cholesterol-saturated bile predisposes to the formation of gall-stones and acts
as an irritant, producing inflammatory changes in the gallbladder.
Four times more women than men develop cholesterol stones and gallbladder disease; the women are usually older than 40, multiparous, and obese. The incidence of stone formation rises in users of oral contraceptives, estrogens, and clofibrate; these substances are known to increase biliary cholesterol saturation. The incidence of stone formation increases with age as a result of increased hepatic secretion of cholesterol and decreased bile acid synthesis. In addition, there is an increased risk because of mal-absorption of bile salts in patients with gastrointestinal disease or T-tube fistula or in those who have had ileal resection or bypass.
The
incidence also increases in people with diabetes.
Clinical Manifestations
Gallstones
may be silent, producing no pain and only mild gastro-intestinal symptoms. Such
stones may be detected incidentally during surgery or evaluation for unrelated
problems.
The patient with gallbladder disease from gallstones may de-velop two types of symptoms: those due to disease of the gall-bladder itself and those due to obstruction of the bile passages by a gallstone. The symptoms may be acute or chronic. Epigastric distress, such as fullness, abdominal distention, and vague pain in the right upper quadrant of the abdomen, may occur. This dis-tress may follow a meal rich in fried or fatty foods.
PAIN AND BILIARY COLIC
If a
gallstone obstructs the cystic duct, the gallbladder becomes distended,
inflamed, and eventually infected (acute cholecystitis). The patient develops a
fever and may have a palpable abdominal mass. The patient may have biliary
colic with excruciating upper right abdominal pain that radiates to the back or
right shoulder, is usually associated with nausea and vomiting, and is
noticeable several hours after a heavy meal. The patient moves about
rest-lessly, unable to find a comfortable position. In some patients the pain
is constant rather than colicky.
Such a
bout of biliary colic is caused by contraction of the gall-bladder, which
cannot release bile because of obstruction by the stone. When distended, the
fundus of the gallbladder comes in contact with the abdominal wall in the
region of the right ninth and tenth costal cartilages. This produces marked
tenderness in the right upper quadrant on deep inspiration and prevents full
in-spiratory excursion.
The
pain of acute cholecystitis may be so severe that analgesics are required.
Morphine is thought to increase spasm of the sphincter of Oddi and may be
avoided in many cases in favor of meperidine (Porth, 2002). This is
controversial because morphine is the preferred analgesic agent for management
of acute pain, and meperidine has metabolites toxic to the CNS.
If the
gallstone is dislodged and no longer obstructs the cystic duct, the gallbladder
drains and the inflammatory process sub-sides after a relatively short time. If
the gallstone continues to ob-struct the duct, abscess, necrosis, and
perforation with generalized peritonitis may result.
JAUNDICE
Jaundice
occurs in a few patients with gallbladder disease and usually occurs with
obstruction of the common bile duct. The bile, which is no longer carried to
the duodenum, is absorbed by the blood and gives the skin and mucous membrane a
yellow color. This is frequently accompanied by marked itching of the skin.
CHANGES IN URINE AND STOOL COLOR
The
excretion of the bile pigments by the kidneys gives the urine a very dark
color. The feces, no longer colored with bile pigments, are grayish, like
putty, and usually described as clay-colored.
VITAMIN DEFICIENCY
Obstruction
of bile flow also interferes with absorption of the fat-soluble vitamins A, D,
E, and K. Therefore, the patient may ex-hibit deficiencies (eg, bleeding caused
by vitamin K deficiency, which interferes with normal blood clotting) of these
vitamins if biliary obstruction has been prolonged.
Assessment and Diagnostic Findings
ABDOMINAL X-RAY
An
abdominal x-ray may be obtained if gallbladder disease is sug-gested to exclude
other causes of symptoms. However, only 15% to 20% of gallstones are calcified
sufficiently to be visible on such x-ray studies.
ULTRASONOGRAPHY
Ultrasonography
has replaced oral cholecystography as the diag-nostic procedure of choice
because it is rapid and accurate and can be used in patients with liver
dysfunction and jaundice. It does not expose patients to ionizing radiation.
The procedure is most accurate if the patient fasts overnight so that the
gallbladder is distended. The use of ultrasound is based on reflected sound
waves. Ultrasonography can detect calculi in the gallbladder or a dilated common
bile duct. It is reported to detect gallstones with 95% accuracy.
RADIONUCLIDE IMAGING OR CHOLESCINTIGRAPHY
Cholescintigraphy is used successfully in the diagnosis of acute
cholecystitis. In this procedure, a radioactive agent is adminis-tered
intravenously. It is taken up by the hepatocytes and excreted rapidly through
the biliary tract. The biliary tract is then scanned, and images of the
gallbladder and biliary tract are obtained. This test is more expensive than
ultrasonography, takes longer to per-form, exposes the patient to radiation,
and cannot detect gall-stones. Its use may be limited to cases in which
ultrasonography is not conclusive.
CHOLECYSTOGRAPHY
Although
it has been replaced by ultrasonography as the test of choice, cholecystography
is still used if ultrasound equipment is not available or if the ultrasound
results are inconclusive. Oral cholangiography may be performed to detect
gallstones and to as-sess the ability of the gallbladder to fill, concentrate
its contents, contract, and empty. An iodide-containing contrast agent excreted
by the liver and concentrated in the gallbladder is administered to the
patient. The normal gallbladder fills with this radiopaque substance. If
gallstones are present, they appear as shadows on the x-ray film.
Contrast
agents include iopanoic acid (Telepaque), iodipamide meglumine (Cholografin),
and sodium ipodate (Oragrafin). These agents are administered orally 10 to 12
hours before the x-ray study. To prevent contraction and emptying of the
gallbladder, the patient is permitted nothing by mouth after the contrast agent
is administered.
The
patient is asked about allergies to iodine or seafood. If no allergy is
identified, the patient receives the oral form of the con-trast agent the
evening before the x-rays are obtained. An x-ray of the right upper abdomen is
obtained. If the gallbladder is found to fill and empty normally and to contain
no stones, gallbladder disease is ruled out. If gallbladder disease is present,
the gallblad-der may not be visualized because of obstruction by gallstones. A
repeat of the oral cholecystogram with a second dose of the con-trast agent may
be necessary if the gallbladder is not visualized on the first attempt.
Cholecystography
in the obviously jaundiced patient is not useful because the liver cannot
excrete the radiopaque dye into the gallbladder in the presence of jaundice.
Oral cholecys-tography is likely to continue to be used as part of the
evaluation of the few patients who have been treated with gallstone dissolu-tion therapy or lithotripsy.
ENDOSCOPIC RETROGRADE CHOLANGIOPANCREATOGRAPHY
Endoscopic retrograde cholangiopancreatography (ERCP)permits direct
visualization of structures that could once be seen only during laparotomy. The
examination of the hepatobiliary system is carried out via a side-viewing
flexible fiberoptic endo-scope inserted into the esophagus to the descending
duodenum (Fig. 40-3). Multiple position changes are required during the
procedure, beginning in the left semiprone position to pass the endoscope.
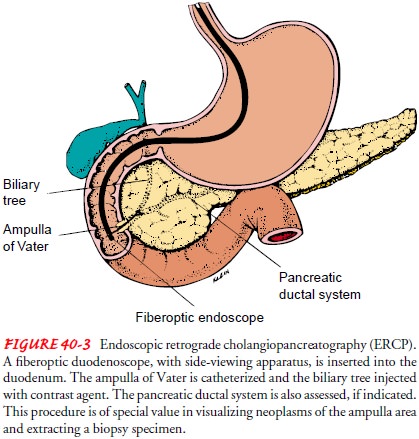
Fluoroscopy
and multiple x-rays are used during ERCP to evaluate the presence and location
of ductal stones. Careful in-sertion of a catheter through the endoscope into
the common bile duct is the most important step in sphincterotomy (division of the
muscles of the biliary sphincter) for gallstone extraction via this technique.
Nursing Implications.
The procedure requires a cooperative pa-tient to permit insertion of the endoscope without damage to the gastrointestinal tract structures, including the biliary tree.
Before the
procedure, the patient is given an explanation of the proce-dure and his or her
role in it. The patient takes nothing by mouth for several hours before the
procedure. Moderate sedation is used with this procedure, so the sedated
patient must be monitored closely. Most endoscopists use a combination of an
opioid and a benzodiazepine. Medications such as glucagon or anticholinergics
may also be necessary to eliminate duodenal peristalsis to make cannulation
easier. The nurse observes closely for signs of respi-ratory and central
nervous system depression, hypotension, over-sedation, and vomiting (if
glucagon is given). During ERCP, the nurse monitors intravenous fluids,
administers medications, and positions the patient.
After
the procedure, the nurse monitors the patient’s condi-tion, observing vital
signs and monitoring for signs of perforation or infection. The nurse also
monitors the patient for side effects of any medications received during the
procedure and for return of the gag and cough reflexes after the use of local
anesthetics.
PERCUTANEOUS TRANSHEPATIC CHOLANGIOGRAPHY
Percutaneous
transhepatic cholangiography involves the injection of dye directly into the
biliary tract. Because of the relatively large concentration of dye that is
introduced into the biliary system, all components of the system, including the
hepatic ducts within the liver, the entire length of the common bile duct, the
cystic duct, and the gallbladder, are outlined clearly.
This
procedure can be carried out even in the presence of liver dysfunction and
jaundice. It is useful for distinguishing jaundice caused by liver disease
(hepatocellular jaundice) from that caused by biliary obstruction, for
investigating the gastrointestinal symp-toms of a patient whose gallbladder has
been removed, for locating stones within the bile ducts, and for diagnosing
cancer involving the biliary system.
This
sterile procedure is performed under moderate sedation on a patient who has
been fasting; the patient receives local anesthesia and intravenous sedation.
Coagulation parameters and platelet count should be normal to minimize the risk
for bleeding. Broad-spectrum antibiotics are administered during the procedure
due to the high prevalence of bacterial coloniza-tion from obstructed biliary
systems. After infiltration with a local anesthetic agent, a flexible needle is
inserted into the liver from the right side in the midclavicular line
immediately be-neath the right costal margin. Successful entry of a duct is
noted when bile is aspirated or upon the injection of a contrast agent.
Ultrasound guidance can be used for duct puncture. Bile is as-pirated and
samples are sent for bacteriology and cytology. A water-soluble contrast agent
is injected to fill the biliary system. The fluoroscopy table is tilted and the
patient repositioned to allow x-rays to be taken in multiple projections.
Delayed x-ray views can identify abnormalities of more distant ducts and
de-termine the length of a stricture or multiple strictures. Before the needle
is removed, as much dye and bile as possible are as-pirated to forestall
subsequent leakage into the needle tract and eventually into the peritoneal
cavity, thus minimizing the risk of bile peritonitis.
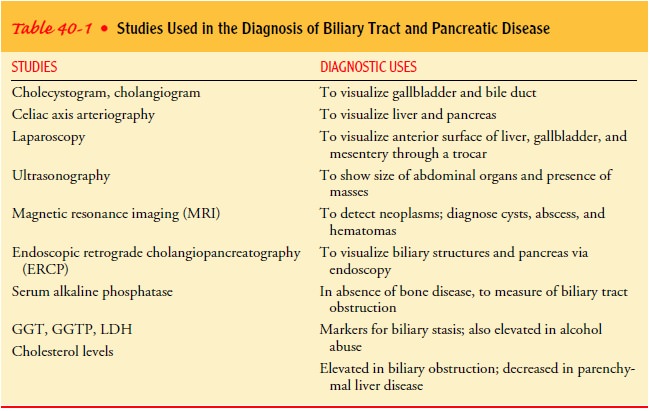
Table
40-1 identifies various procedures and their diagnostic uses.
Medical Management
The
major objectives of medical therapy are to reduce the inci-dence of acute
episodes of gallbladder pain and cholecystitis by supportive and dietary
management and, if possible, to remove the cause of cholecystitis by
pharmacologic therapy, endoscopic procedures, or surgical intervention.
Although nonsurgical approaches have the advantage of elim-inating risks associated with surgery, they are associated with per-sistent symptoms or recurrent stone formation. Most of the nonsurgical approaches, including lithotripsy and dissolution of gallstones, provide only temporary solutions to the problems as-sociated with gallstones. They are therefore rarely used in the United States. In some instances, other treatment approaches may be indicated; these are described below.
Removal
of the gallbladder (cholecystectomy)
through tradi-tional surgical approaches was considered the standard approach
to management for more than 100 years. However, dramatic changes have occurred
in the surgical management of gallbladder disease. There is now widespread use
of laparoscopic cholecys-tectomy (removal
of the gallbladder through a small incisionthrough the umbilicus). As a result,
surgical risks have decreased, along with the length of hospital stay and the
long recovery pe-riod associated with the standard surgical cholecystectomy.
NUTRITIONAL AND SUPPORTIVE THERAPY
Approximately
80% of the patients with acute gallbladder inflam-mation achieve remission with
rest, intravenous fluids, nasogastric suction, analgesia, and antibiotic
agents. Unless the patient’s con-dition deteriorates, surgical intervention is
delayed until the acute symptoms subside and a complete evaluation can be
carried out.
The
diet immediately after an episode is usually limited to low-fat liquids. The
patient can stir powdered supplements high in protein and carbohydrate into
skim milk. Cooked fruits, rice or tapioca, lean meats, mashed potatoes, non–gas-forming
veg-etables, bread, coffee, or tea may be added as tolerated. The pa-tient
should avoid eggs, cream, pork, fried foods, cheese and rich dressings,
gas-forming vegetables, and alcohol. It is important to remind the patient that
fatty foods may bring on an episode. Di-etary management may be the major mode
of therapy in patients who have had only dietary intolerance to fatty foods and
vague gastrointestinal symptoms (Dudek, 2001).
PHARMACOLOGIC THERAPY
Ursodeoxycholic
acid (UDCA) and chenodeoxycholic acid (che-nodiol or CDCA) have been used to
dissolve small, radiolucent gallstones composed primarily of cholesterol. UDCA
has fewer side effects than chenodiol and can be administered in smaller doses
to achieve the same effect. It acts by inhibiting the synthe-sis and secretion
of cholesterol, thereby desaturating bile. Exist-ing stones can be reduced in
size, small ones dissolved, and new stones prevented from forming. Six to 12
months of therapy are required in many patients to dissolve stones, and monitoring
of the patient is required during this time. The effective dose of medication
depends on body weight. This method of treatment is generally indicated for
patients who refuse surgery or for whom surgery is considered too risky.
Patients
with significant, frequent symptoms, cystic duct oc-clusion, or pigment stones
are not candidates for this therapy. Symptomatic patients with acceptable
operative risk are more ap-propriate for laparoscopic or open cholecystectomy.
NONSURGICAL REMOVAL OF GALLSTONES
Dissolving Gallstones.
Several
methods have been used to dis-solve gallstones by infusion of a solvent
(mono-octanoin or methyl tertiary butyl ether [MTBE]) into the gallbladder. The
solvent can be infused through the following routes: a tube or catheter
inserted percutaneously directly into the gallbladder; a tube or drain inserted
through a T-tube tract to dissolve stones not removed at the time of surgery;
an ERCP endoscope; or a transnasal biliary catheter.
In the
last procedure, the catheter is introduced through the mouth and inserted into
the common bile duct. The upper end of the tube is then rerouted from the mouth
to the nose and left in place. This enables the patient to eat and drink
normally while passage of stones is monitored or chemical solvents are infused
to dissolve the stones. This method of dissolution of stones is not widely used
in patients with gallstone disease.
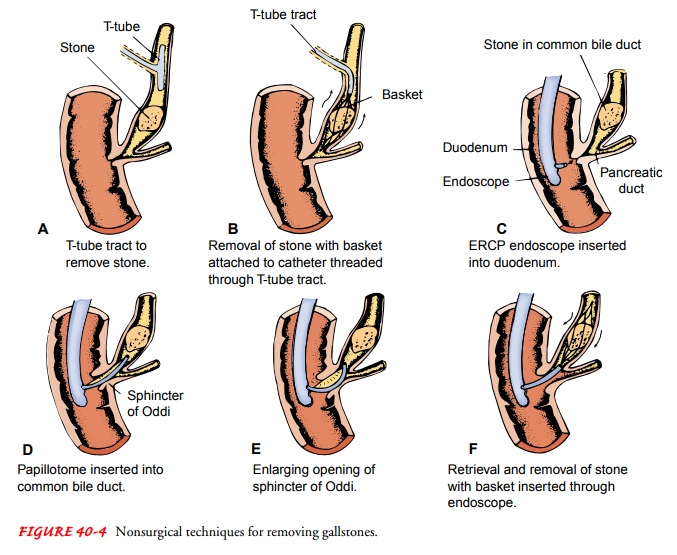
Stone Removal by Instrumentation.
Several
nonsurgical meth-ods are used to remove stones that were not removed at the
time of cholecystectomy or have become lodged in the common bile duct (Fig.
40-4A, B). A catheter and instrument
with a basket at-tached are threaded through the T-tube tract or fistula formed
at the time of T-tube insertion; the basket is used to retrieve and re-move the
stones lodged in the common bile duct.
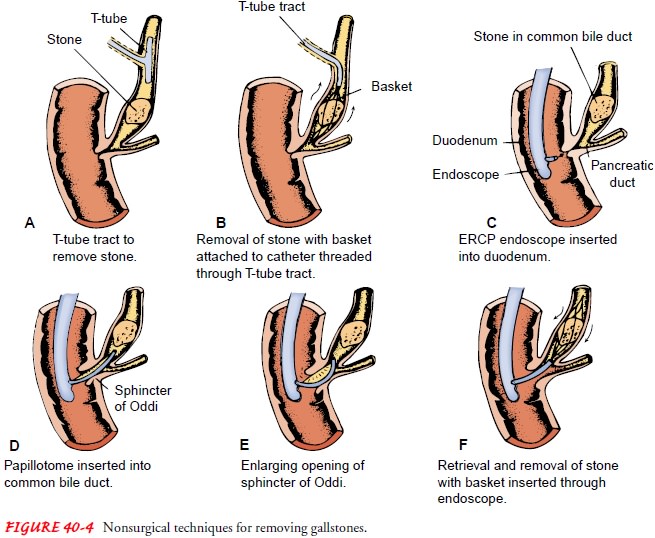
A
second procedure involves the use of the ERCP endoscope (see Fig. 40-4C ). After the endoscope is inserted, a
cutting in-strument is passed through the endoscope into the ampulla of Vater
of the common bile duct. It may be used to cut the sub-mucosal fibers, or
papilla, of the sphincter of Oddi, enlarging the opening, which may allow the
lodged stones to pass spontaneously into the duodenum. Another instrument with
a small basket or balloon at its tip may be inserted through the endoscope to
retrieve the stones (see Fig. 40-4D–F
). Although complications after this procedure are rare, the patient must be
observed closely for bleed-ing, perforation, and the development of
pancreatitis or sepsis.
The
ERCP procedure is particularly useful in the diagnosis and treatment of
patients who have symptoms after biliary tract surgery, for patients with
intact gallbladders, and for patients in whom surgery is particularly
hazardous.
Extracorporeal Shock-Wave Lithotripsy.
Extracorporeal
shock-wave therapy (lithotripsy or ESWL) has been used for nonsurgi-cal
fragmentation of gallstones. The word lithotripsy
is derived from lithos, meaning
stone, and tripsis, meaning rubbing
or fric-tion. This noninvasive procedure uses repeated shock waves di-rected at
the gallstones in the gallbladder or common bile duct to fragment the stones.
The energy is transmitted to the body through a fluid-filled bag, or it may be
transmitted while the pa-tient is immersed in a water bath. The converging
shock waves are directed to the stones to be fragmented.
After
the stones are gradually broken up, the stone fragments pass from the
gallbladder or common bile duct spontaneously, are removed by endoscopy, or are
dissolved with oral bile acid or solvents. Because the procedure requires no
incision and no hos-pitalization, patients are usually treated as outpatients,
but several sessions are generally necessary.
The
advent of laparoscopic cholecystectomy has reduced the use of this method to
treat gallbladder stones. It is used in some centers for a small percentage of
suitable patients (those with common bile duct stones who may not be surgical
candidates), sometimes in combination with dissolution therapy.
Intracorporeal Lithotripsy.
Stones in the gallbladder or commonbile duct may be fragmented by means of laser pulse technology. A laser pulse is directed under fluoroscopic guidance with the use of devices that can distinguish between stones and tissue. The laser pulse produces rapid expansion and disintegration of plasma on the stone surface, resulting in a mechanical shock wave. Electro-hydraulic lithotripsy uses a probe with two electrodes that deliver electric sparks in rapid pulses, creating expansion of the liquid environment surrounding the gallstones. This results in pressure waves that cause stones to fragment. This technique can be em-ployed percutaneously with the use of a basket or balloon catheter system or by direct visualization through an endoscope. Repeated procedures may be necessary due to stone size, local anatomy, bleeding, or technical difficulty. A nasobiliary tube can be inserted to allow for biliary decompression and prevent stone impaction in the common bile duct. This approach allows time for improve-ment in the patient’s clinical condition until gallstones are cleared endoscopically, percutaneously, or surgically.
SURGICAL MANAGEMENT
Surgical
treatment of gallbladder disease and gallstones is carried out to relieve
persistent symptoms, to remove the cause of biliary colic, and to treat acute
cholecystitis. Surgery may be delayed until the patient’s symptoms have
subsided or may be performed as an emergency procedure if the patient’s
condition necessitates it.
Preoperative Measures.
A chest
x-ray, electrocardiogram, andliver function tests may be performed in addition
to x-ray studies of the gallbladder. Vitamin K may be administered if the
pro-thrombin level is low. Blood component therapy may be admin-istered before
surgery. Nutritional requirements are considered; if the nutritional status is
suboptimal, it may be necessary to pro-vide intravenous glucose with protein
hydrolysate supplements to aid wound healing and help prevent liver damage.
Preparation
for gallbladder surgery is similar to that for any upper abdominal laparotomy
or laparoscopy. Instructions and explanations are given before surgery with
regard to turning and deep breathing. Pneumonia and atelectasis are possible
postoper-ative complications that can be avoided by deep-breathing exer-cises
and frequent turning. The patient should be informed that drainage tubes and a
nasogastric tube and suction may be re-quired during the immediate
postoperative period if an open cholecystectomy is performed.
Laparoscopic Cholecystectomy.
Laparoscopic
cholecystectomy(Fig. 40-5) has dramatically changed the approach to the
man-agement of cholecystitis. It has become the new standard for ther-apy of
symptomatic gallstones. Approximately 700,000 patients in the United States
require surgery each year for removal of the gallbladder, and 80% to 90% of
them are candidates for laparo-scopic cholecystectomy (Bornman &
Beckingham, 2001). If the common bile duct is thought to be obstructed by a
gallstone, an ERCP with sphincterotomy may be performed to explore the duct
before laparoscopy.
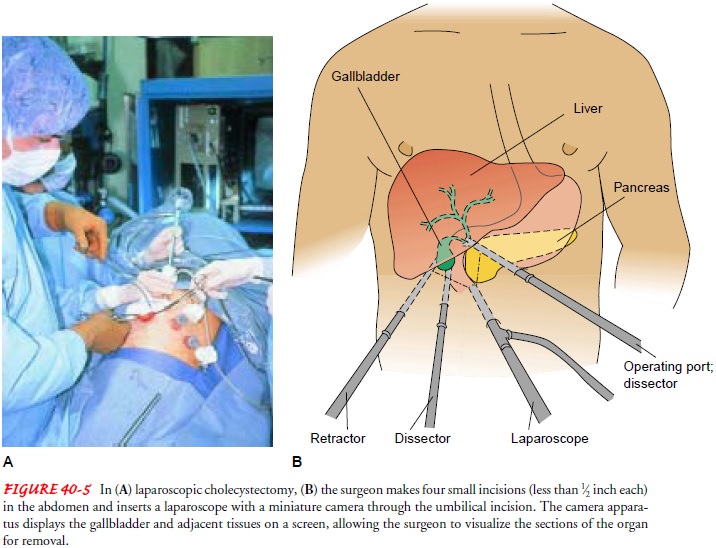
Before
the procedure, the patient is informed that an open ab-dominal procedure may be
necessary, and general anesthesia is administered. Laparoscopic cholecystectomy
is performed through a small incision or puncture made through the abdominal
wall in the umbilicus. The abdominal cavity is insufflated with carbon dioxide
(pneumoperitoneum) to assist in inserting the laparo-scope and to aid the
surgeon in visualizing the abdominal struc-tures. The fiberoptic scope is
inserted through the small umbilical incision. Several additional punctures or
small incisions are made in the abdominal wall to introduce other surgical
instruments into the operative field. The surgeon visualizes the biliary system
through the laparoscope; a camera attached to the scope permits a view of the
intra-abdominal field to be transmitted to a televi-sion monitor. After the
cystic duct is dissected, the common bile duct is imaged by ultrasound or
cholangiography to evaluate the anatomy and identify stones. The cystic artery
is dissected free and clipped. The gallbladder is separated away from the
hepatic bed and dissected. The gallbladder is then removed from the ab-dominal
cavity after bile and small stones are aspirated. Stone for-ceps also can be
used to remove or crush larger stones.
The
advantage of the laparoscopic procedure is that the pa-tient does not
experience the paralytic ileus that occurs with open abdominal surgery and has
less postoperative abdominal pain. The patient is often discharged from the
hospital on the day of surgery or within a day or two and can resume full
activity and employment within a week of the surgery.
Conversion to a traditional abdominal surgical procedure may be necessary if problems are encountered during the laparoscopic procedure; this occurs in 2% to 8% of reported surgical cases.
Conversion
is required more often, approximately 20% of the time, in those with acute
cholecystitis (Lai et al., 1998). Careful screening of patients and
identification of those at low risk for complications limits the frequency of
conversion to an open ab-dominal procedure. With wider use of laparoscopic
procedures, however, there may be an increase in the number of such con-versions.
The most serious complication after laparoscopic chole-cystectomy is a bile
duct injury.
Because
of the short hospital stay, it is important to provide written as well as
verbal instructions about managing postopera-tive pain and reporting signs and
symptoms of intra-abdominal complications, including loss of appetite,
vomiting, pain, disten-tion of the abdomen, and temperature elevation. Although
re-covery from laparoscopic cholecystectomy is rapid, patients are drowsy
afterward. The nurse must ensure that the patient has as-sistance at home
during the first 24 to 48 hours. If pain occurs in the right shoulder or
scapular area (from migration of the CO2 used to insufflate the abdominal cavity
during the procedure), the nurse may recommend use of a heating pad for 15 to
20 minutes hourly, walking, and sitting up when in bed.
Cholecystectomy.
In this
procedure, the gallbladder is removedthrough an abdominal incision (usually
right subcostal) after the cystic duct and artery are ligated. The procedure is
performed for acute and chronic cholecystitis. In some patients a drain may be
placed close to the gallbladder bed and brought out through a punc-ture wound
if there is a bile leak. The drain type is chosen based on the physician’s
preference. A small leak should close spontaneously in a few days with the
drain preventing accumulation of bile. Usu-ally only a small amount of
serosanguinous fluid will drain in the initial 24 hours after surgery, and then
the drain will be removed.
The drain is usually maintained if there is
excess oozing or bile leak-age. Use of a T-tube inserted into the common bile
duct during the open procedure is now uncommon; it is used only in the setting
of a complication (ie, retained common bile duct stone). Bile duct in-jury is a
serious complication of this procedure but occurs less fre-quently than with
the laparoscopic approach. Once one of the most common surgical procedures in
the United States, this procedure has largely been replaced by laparoscopic
cholecystectomy.
Mini-cholecystectomy.
Mini-cholecystectomy
is a surgical pro-cedure in which the gallbladder is removed through a small
inci-sion. If needed, the surgical incision is extended to remove large
gallbladder stones. Drains may or may not be used. The cost sav-ings resulting
from the shorter hospital stay have been `identified as a major reason for
pursuing this type of procedure. Debate ex-ists about this procedure because it
limits exposure to all the in-volved biliary structures.
Choledochostomy.
Choledochostomyinvolves an
incision intothe common duct, usually for removal of stones. After the stones
have been evacuated, a tube usually is inserted into the duct for drainage of
bile until edema subsides. This tube is connected to gravity drainage tubing.
The gallbladder also contains stones, and as a rule a cholecystectomy is
performed at the same time.
Surgical Cholecystostomy.
Cholecystostomyis performed
whenthe patient’s condition prevents more extensive surgery or when an acute
inflammatory reaction is severe. The gallbladder is surgically opened, the
stones and the bile or the purulent drainage are removed, and a drainage tube
is secured with a purse-string suture. The drainage tube is connected to a
drainage system to prevent
bile from leaking around the tube or escaping into the peritoneal cavity. After
recovery from the acute episode, the pa-tient may return for cholecystectomy.
Despite its lower risk, sur-gical cholecystostomy has a high mortality rate
(reported as high as 20% to 30%) because of the underlying disease process.
Percutaneous Cholecystostomy.
Percutaneous
cholecystostomyhas been used in the treatment and diagnosis of acute
cholecysti-tis in patients who are poor risks for any surgical procedure or for
general anesthesia. These may include patients with sepsis or se-vere cardiac,
renal, pulmonary, or liver failure. Under local anes-thesia, a fine needle is
inserted through the abdominal wall and liver edge into the gallbladder under
the guidance of ultrasound or computed tomography. Bile is aspirated to ensure
adequate placement of the needle, and a catheter is inserted into the
gall-bladder to decompress the biliary tract. Almost immediate relief of pain
and resolution of signs and symptoms of sepsis and chole-cystitis have been
reported with this procedure. Antibiotic agents are administered before,
during, and after the procedure.
Gerontologic Considerations
Surgical
intervention for disease of the biliary tract is the most common operative
procedure performed in the elderly. Choles-terol saturation of bile increases
with age due to increased hepatic secretion of cholesterol and decreased bile
acid synthesis.
Although
the incidence of gallstones increases with age, the el-derly patient may not
exhibit the typical picture of fever, pain, chills, and jaundice. Symptoms of
biliary tract disease in the el-derly may be accompanied or preceded by those
of septic shock, which include oliguria, hypotension, changes in mental status,
tachycardia, and tachypnea.
Although
surgery in the elderly presents a risk because of pre-existing associated
diseases, the mortality rate from serious com-plications from biliary tract
disease itself is also high. The risk of death and complications is increased
in the elderly patient who undergoes emergency surgery for life-threatening
disease of the biliary tract. Despite chronic illness in many elderly patients,
elec-tive cholecystectomy is usually well tolerated and can be carried out with
low risk if expert assessment and care are provided be-fore, during, and after
the surgical procedure.
Because
of recent changes in the health care system, there has been a decrease in the
number of elective surgical procedures performed, including cholecystectomies.
As a result, patients requiring the procedure are seen in the later stages of
disease. Simultaneously, patients undergoing surgery are increasingly older
than 60 years of age and have complicated acute cholecys-titis. The higher risk
of complications and shorter hospital stays make it essential that older
patients and their family members re-ceive specific information about signs and
symptoms of compli-cations and measures to prevent them.
Related Topics