Chapter: Medical Surgical Nursing: End-of-Life Care
Providing Culturally Sensitive Care at the End of Life - Nursing Care of the Terminally Ill Patient
PROVIDING CULTURALLY SENSITIVE CARE AT THE END OF LIFE
Although
death, grief, and mourning are universally accepted as-pects of living, values,
expectations, and practices during serious illness, as death approaches, and
following death are culturally bound and expressed. Health care providers may
share very sim-ilar values concerning end-of-life care and may find that they
are inadequately prepared to assess for and implement care plans that support
culturally diverse perspectives. Historical mistrust of the health care system
and unequal access to even basic medical care may underlie the beliefs and
attitudes among ethnically di-verse populations (Crawley, Payne, Bolden et al.,
2000; Phipps, True & Pomerantz, 2000). In addition, lack of education or
knowl-edge concerning end-of-life care treatment options and language barriers
influence decisions among many socioeconomically dis-advantaged groups.
Much of the formal structure concerning
health care decisions in the United States is rooted in the Western notions of
auton-omy, truth telling, and the acceptability of withdrawing or with-holding
life-prolonging medical treatment at the end of life. Yet in many cultures,
interdependence is valued over autonomy, leading to decision and communication
styles that favor relin-quishment of decision making to family members or to a
per-ceived authority figure, such as the physician (Blackhall et al., 1995;
Ersek, Kagawa-Singer, Barnes et al., 1998). In addition, there is variation in
preference regarding the use of life-prolonging medical treatments such as
cardiopulmonary resuscitation and artificially provided nutrition and hydration
at the end of life; some groups are less likely to agree with withholding or
with-drawing such life support in terminal illness (Caralis, Davis, Wright et
al., 1993).
The nurse’s role is to assess the values, preferences, and prac-tices of every patient, regardless of ethnicity, socioeconomic sta-tus, or background. The nurse can share knowledge about the patient’s and family’s cultural beliefs and practices with the health care team and facilitate the adaptation of the care plan to accom-modate these practices. For example, the nurse may find that a patient prefers to have his eldest son make all of his care decisions. Institutional practices and laws governing informed consent are also rooted in the Western notion of autonomous decision making and informed consent. If a patient who wishes to defer decisions to his son, the nurse can work with the team to negotiate in-formed consent, respecting the patient’s right not to participate in decision making and honoring his family’s cultural practices (Ersek et al., 1998).
The
nurse should assess and document the patient’s and fam-ily’s specific beliefs,
preferences, and practices regarding end-of-life care, preparation for death,
and after-death rituals. Chart 17-4 identifies topics that the nurse should
cover and questions that the nurse may use to elicit the information. The nurse
must use judgment and discretion about the timing and setting for elicit-ing
this information. Some patients may wish to have a family member speak for them
or because of advanced illness may be un-able to provide information. The nurse
should give the patient and family a context for the discussion, such as “It is
very impor-tant to us to provide care that addresses your needs and the needs
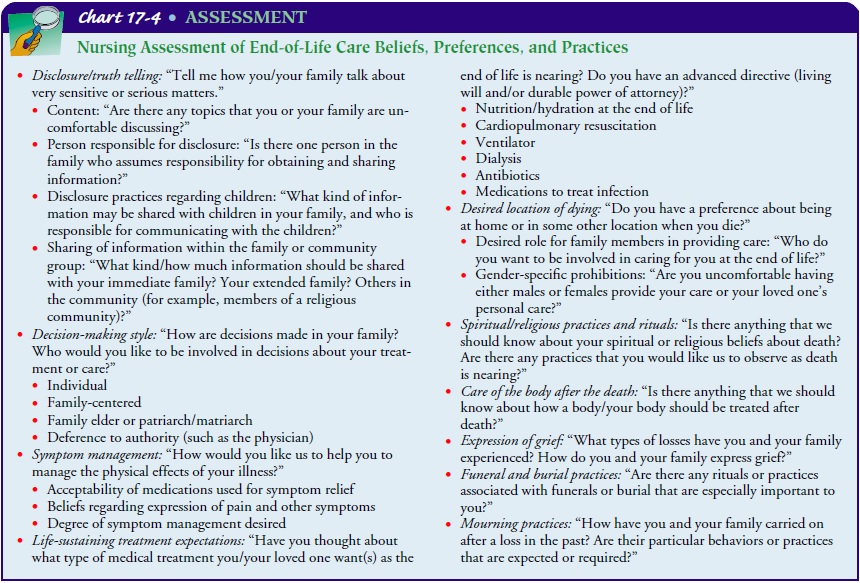
of your family. We want to honor and support your wishes, and want you to feel free to tell us how we are doing, and what we could do to better meet your needs. I’d like to ask you some ques-tions; what you tell me will help me to understand and support what is most important to you at this time. You don’t need to an-swer anything that makes you uncomfortable. Is it all right to ask some questions?” The assessment of end-of-life beliefs, prefer-ences, and practices will probably need to be carried out in short segments over a period of time (for example, across multiple days of an inpatient hospital stay or in conjunction with multiple pa-tient visits to an outpatient setting). The novice nurse’s discom-fort with asking questions and discussing this type of sensitive content can be reduced by prior practice in a classroom or clin-ical skills laboratory, observation of interviews conducted by experienced nurses, and partnering with an experienced nurse during the first few assessments.
Related Topics