Chapter: Medical Microbiology: An Introduction to Infectious Diseases: Streptococci and Enterococci
Pneumococcal Disease
PNEUMOCOCCAL DISEASE
The most common form of infection with S. pneumoniae is pneumonia, which begins with fever and a shaking chill followed by signs that localize the disease to the lung. These include difficulty breathing and cough with production of purulent sputum, sometimes containing blood. The pneumonia typically fills part or all of a lobe of the lung with inflammatory cells, and the bacteria may spread to the blood-stream and thus other organs. The most important of the latter is the central nervous system, where seeding with pneumococci leads to acute purulent meningitis.
EPIDEMIOLOGY
S. pneumoniae is a leading cause of pneumonia, acute purulent meningitis, bacteremia,and other invasive infections. In the United States it is responsible for an estimated 3000 cases of meningitis, 50,000 cases of bacteremia, and 500,000 cases of pneumonia each year. Worldwide, more than 5 million children die every year from pneumococcal dis-ease. S. pneumoniae is also the most frequent cause of otitis media , a virtually universal disease of childhood with millions of cases every year. Pneumococcal infections occur throughout life but are most common in the very young ( <2 years) and in the old ( >60 years). Alcoholism, diabetes mellitus, chronic renal disease, asple-nia, and some malignancies are all associated with more frequent and serious pneumo-coccal infection.
Infections are derived from colonization of the nasopharynx, where pneumococci can be found in 5 to 40% of healthy persons depending on age, season, and other factors. The highest rates are among children in the winter. Respiratory secretions containing pneumococci may be transmitted from person to person by direct contact or from the microaerosols created by coughing and sneezing in close quarters. Such conditions are fa-vored by crowded living conditions, particularly when colonized persons are mixed with susceptible ones, as in child care centers, recruitment barracks, and prisons. As with other bacterial pneumonias, viral respiratory infection and underlying chronic disease are im-portant predisposing factors.
About 23 of the 90 pneumococcal serotypes produce disease more often than the others. There is also a variation in the age and geographic distribution of cases. These differences are presumably due to enhanced virulence factors in these types, but the spe-cific reasons are not known. These features do not influence the medical management of individual cases but are important in devising prevention strategies such as immuniza-tion .
PATHOGENESIS
Pneumococcal adherence to nasopharyngeal cells involves multiple factors. The primary relationship is the bridging effect of the choline binding protein’s attachment to cell wall cholines and carbohydrates covering or exposed on the surface of host epithelial cells. This binding may be aided by the exposure of additional receptors by neuraminidase di-gestion or pneumolysin stimulated cytokine activation of host cells. Aspiration of respi-ratory secretions containing these pneumococci is the initial event leading to pneumonia. This must be a common event. Normally, aspirated organisms are cleared rapidly by the defense mechanisms of the lower respiratory tract, including the cough and epiglottic re-flexes; the mucociliary “blanket;” and phagocytosis by alveolar macrophages. Host fac-tors that impair the combined efficiency of these defenses can allow pneumococci to reach the alveoli and multiply there. These include chronic pulmonary diseases; damage to bronchial epithelium from smoking or air pollution; and respiratory dysfunction from alcoholic intoxication, narcotics, anesthesia, and trauma.
When organisms reach the alveolus, the involvement of pneumococcal virulence fac-tors appears to operate in two stages. The first stage is early in infection, when the surface capsule of intact organisms acts to block phagocytosis by complement inhibition. This al-lows the organisms to multiply and spread despite an acute inflammatory response. The second stage occurs when organisms begin to disintegrate and release a number of factors either synthesized by the pneumococcus or part of its structure, thus causing injury. These include pneumolysin, autolysin, and components of the cell wall.
Capsule
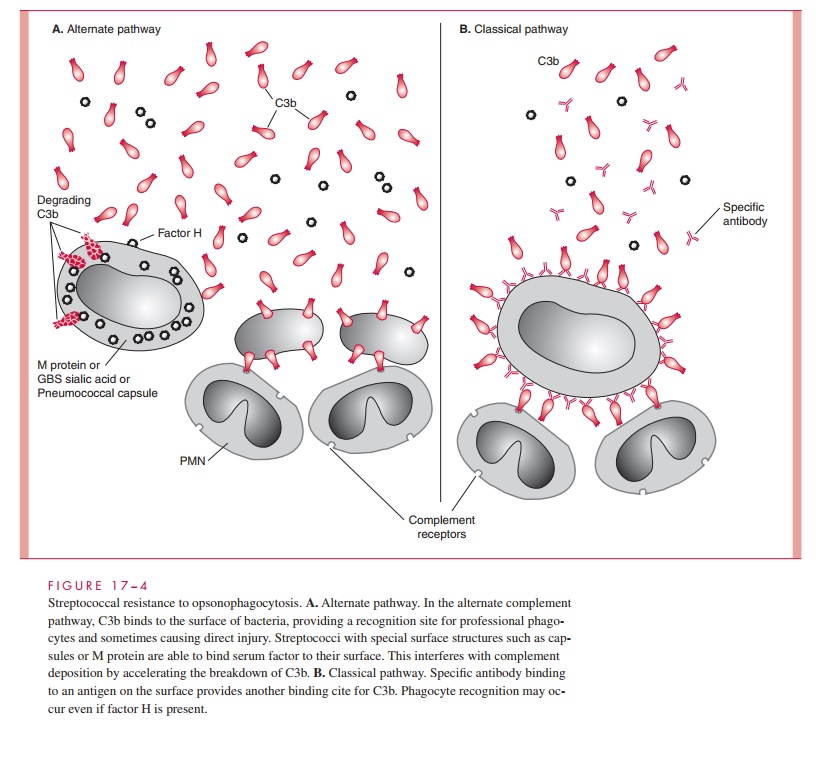
The polysaccharide capsule of S. pneumoniae is the major determinant of virulence. Un-encapsulated mutants do not produce disease in humans or laboratory animals. Like the GBS capsule, pneumococcal polysaccharide interferes with effective deposition of com-plement on the organism’s surface and thus phagocyte recognition and engulfment. This property is particularly important in the absence of specific antibody, when alternate path-way is the primary means for C3b mediated opsonization. The exact mechanism for inter-ference with C3b deposition (see Fig 17 – 4) may differ in detail with that of GBS sialic acid and between the capsular polysaccharide polymers of individual pneumococcal serotypes. The net effect is that the complement fragments recognized by phagocyte receptors are not available on the surface of the organism. When antibody binds to the capsular polysaccharide, C3b generated by the classical pathway binds and opsonophago-cytosis proceeds efficiently.
Pneumolysin
Some of the clinical features seen in the course of pneumococcal infections are not explainable by the capsule alone. These include the dramatic abrupt onset, toxicity, fulmi-nant course, and disseminated intravascular coagulation seen in some cases. Pneu-molysin’s toxicity for pulmonary endothelial cells and direct effect on cilia contributes to the disruption of the endothelial barrier and facilitates the access of pneumococci to the alveoli and eventually their spread beyond into the bloodstream. Pneumolysin also has di-rect effects on phagocytes and suppresses host inflammatory and immune functions. In-jection of purified pneumolysin into the lung of rats causes all of the salient histologic hallmarks of pneumococcal pneumonia. Because pneumolysin is not actively secreted outside the bacterial cell, the action of the autolysins is required to release it.
Other Virulence Determinants
Although the search for the host epithelial cell’s adhesin has been unrewarding, it seems logical that one or more of the surface proteins attached to cell wall teichoic acid are in-volved. Pneumococcal surface protein A (PspA) is found in virtually all pneumococci and has been shown to interfere with complement deposition. In addition to its role in attach-ment, neuraminidase may have a role at other stages of disease. Peptidoglycan and tei-choic acid components of the cell wall have been shown to stimulate inflammation and cerebral edema in experimental meningitis and may do so at other stages of infection. Along with pneumolysin, these may be responsible for the heightened acute inflammatory response seen in pneumococcal infection, which of itself may be destructive to the host.
The combined effects of pneumococcal and host factors produce a pneumonia, which progresses through a series of stages. Initial alveolar multiplication produces a profuse outpouring of serous edema fluid, which is then followed by an influx of poly-morphonuclear leukocytes (PMNs) and erythrocytes (red blood cells; RBCs). By the sec-ond or third day of illness, the lung segment has increased three- to fourfold in weight through accumulation of this cellular, hemorrhagic fluid typically in a single lobe of the lung. In the consolidated alveoli, neutrophils predominate initially, but once actively growing pneumococci are no longer present, macrophages replace the granulocytes and resolution of the lesion ensues. A remarkable feature of pneumococcal pneumonia is the lack of structural damage to the lung, which usually leads to complete resolution on recovery.
IMMUNITY
Immunity to S. pneumoniae infection is provided by antibody directed against the specific pneumococcal capsular type. When antibody binds to the capsular surface, C3b is de-posited by classical pathway mechanisms, and phagocytosis can proceed. Because the number of serotypes is large, complete immunity through natural experience is not realis-tic, which is why pneumococcal infections occur throughout life. Infections are most often seen in the very young, when immunologic experience is minimal, and in the elderly, when immunity begins to wane and risk factors are more common. Antibodies to surface pro-teins and enzymes, including pneumolysin, are also formed in the course of disease, but their role in immunity is unknown.
Related Topics