Chapter: Ophthalmology: Ocular Motility and Strabismus
Diagnosis of Concomitant Strabismus
Diagnosis of Concomitant Strabismus
Evaluating Ocular Alignment with a Focused Light
This is a fundamental examination and is usually the first one performed by the ophthalmologist in patients with suspected concomitant strabismus. The examiner holds the light beneath and close to his or her own eyes and observes the light reflexes on the patient’s corneas (Hirschberg’s method) in near fixation at a distance of 30 cm. Normally, these reflexes are symmetrical. Strabismus is present if the corneal reflex deviates in one eye. The corneal reflexes are symmetrical in normal binocular vision or pseudostrabismus; in esotropia, exotropia, and vertical deviation, they are asymmetrical.
Diagnosis of Infantile Strabismic Amblyopia (Preferential Looking Test)
Strabismus occurs most frequently in the
newborn and infants and must also be treated at this age to minimize the risk
of visual impairment. As the examiner cannot rely on patient cooperation at
this age, examination tech-niques requiring minimal patient cooperation are
necessary. The preferential looking test can be used for early evaluation of
vision beginning at the age of four to six months. This test cannot reliably
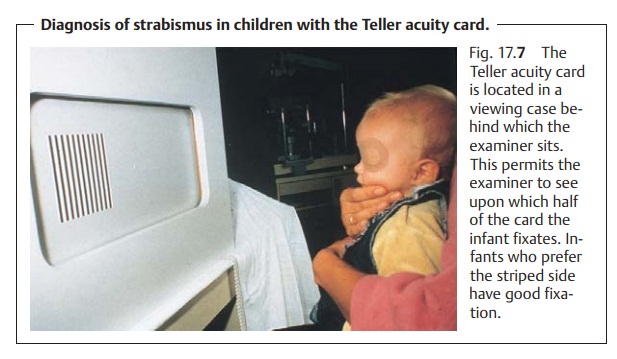
detect strabismic amblyopia. However, Teller acuity cards (Fig. 17.7) are sufficiently
sensitive for early detection of deficits in the presence of defects of the entire visual system.
Procedure:
The infant is shown a card (Teller acuity card) with the
samebackground brightness. The examiner is hidden behind a viewing case that
covers him or her from the front and side. An observation pinhole in the middle
of the card permits the examiner to observe only the infant’s eyes and
determine upon which side of the card the infant is fixating. Infants who
pre-fer the striped side have good fixation.
Diagnosis of Unilateral and Alternating Strabismus (Unilateral Cover Test)
A unilateral cover test can distinguish
between manifest unilateral stra-bismus and alternating strabismus. The patient
is requested to fixate on a point. The examiner than covers one eye and
observes the uncovered eye (Fig. 17.8a – c).
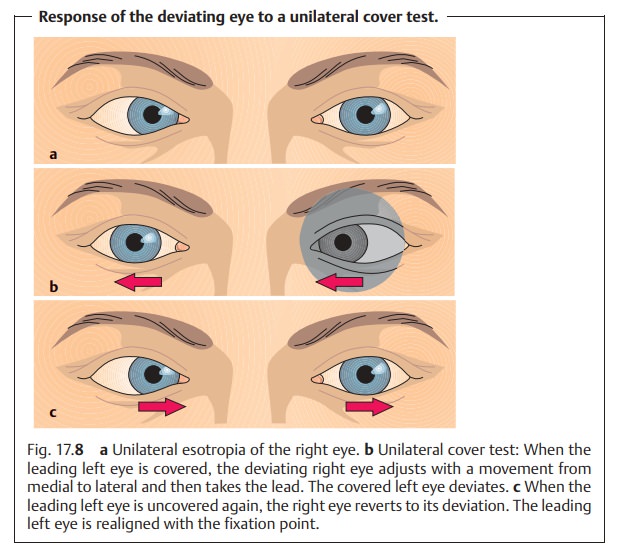
❖Inunilateral strabismus, the same
eye always deviates. When the deviat-ing eye is covered, the uncovered eye
(the leading, nondeviating eye) remains focused on the point of fixation. When
the nondeviating eye is covered, the uncovered deviating eye has to take the
lead. To do so, it will first make a visible adjustment. In esotropia, this
adjustment is from medial to lateral; in exotropia, it is from lateral to
medial.
❖Inbilateral alternating strabismus,both eyes will alternately fixate and deviate.
Measuring the Angle of Deviation
Exact measurement of the angle of deviation is
crucial to prescribing the proper prism correction to compensate for the angle
of deviation and to the corrective surgery that usually follows. A measurement
error may lead to undercorrection or overcorrection of the angle of deviation
during the opera-tion. Example:
Esotropia of + 15 degrees is corrected by shifting the medial rectus 4.0 mm
posteriorly and shortening the lateral rectus 5.0 mm.
The angle of deviation is measured with a cover test in combination withthe use of prism lens of various
refractive powers. The patient fixates on acertain point with the leading eye at a distance of 5 m or 30
cm, depending on which angle of deviation is to be measured. The examiner place
prism lenses of different refractive power before the patient’s deviant eye
until the eye no longer makes any adjustment. This is the case when the angle
of deviation corresponds to the strength of the respective prism and is fully
compensated for by that prism. The tip of the prism must always point in the
direction of deviation during the examination.
Prism bars simplify the examination. These bars contain a series of
prismsof progressively increasing strength arranged one above the other.
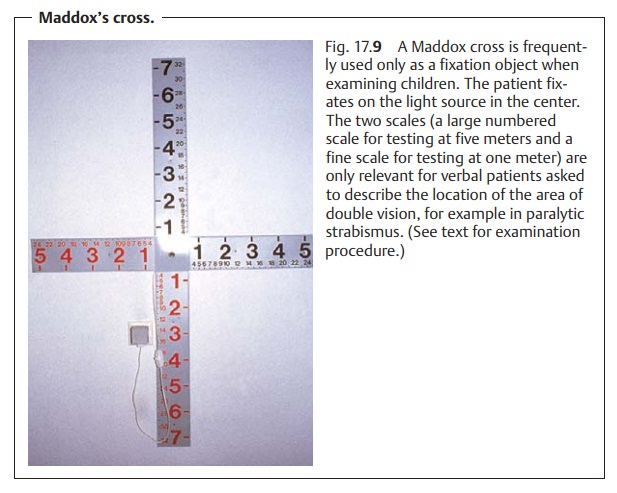
Maddox’s cross (Fig. 17.9) is a device often used to measure the angle ofdeviation. A light source mounted in the center of the cross serves as a fixa-tion point. The patient fixates the light source with his or her leading eye. The objective angle of deviation is measured with prisms as described above. Inchildren, often only the objective angle of deviation is measured as this measurement does not require any action on the part of the patient except for fixating a certain point, in this case the light source at center of the cross. In adults, the examiner can ask the patient to describe the location of the area ofdouble vision (double vision may be a sequela of paralytic strabismus, whichis the most common form encountered in adults). This uses the graduations on the Maddox’s cross. The cross has two scales, a large numbered scale for testing at five meters and a fine scale for testing at one meter (see Fig. 17.9). The patient describes the location of the area of double vision according to a certain number on this scale. The examiner selects the appropriate prism cor-rection according to the patient’s description to correct the angle of deviation of the paralyzed eye. This superimposes the images seen by the deviating eye and the nondeviating eye to eliminate the double vision.
The angle of deviation can be measured in
prism diopters or degrees. One prism diopter refracts light rays approximately
half a degree so that two prism diopters correspond to one degree.
Determining the Type of Fixation
This examination is used to ascertain which part of the retina of the deviatingeye
the image of the fixated point falls on. The patient looks through a
specialophthalmoscope and fixates on a small star that is imaged on the fundus
of the eye. The examiner observes the fundus.
❖Incentral fixation, the image of the star falls on the fovea centralis.
❖Ineccentric fixation, the image of the star falls on an area of the retina out-
side the fovea (Fig. 17.10). Usually this point lies between the fovea and the optic disk.
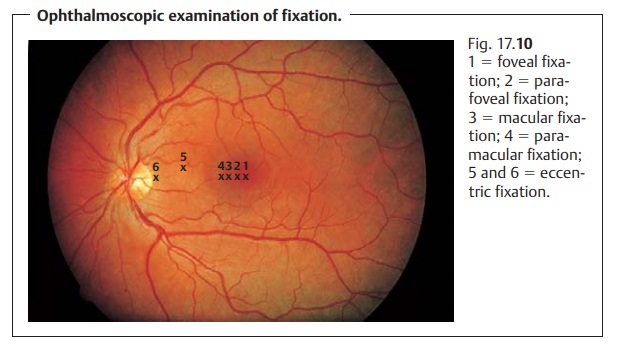
Aside from the type of fixation, one can also
estimate potential visual acuity. The
greater the distance between where the point of fixation lies and the fovea,
the lower the resolving power of the retina and the poorer visual acuity will
be. Initial treatment consists of occlusion therapy to shift an eccentric point
of fixation on to the fovea centralis.
Testing Binocular Vision
Bagolini test:
This test uses flat lenses with fine parallel striations. The stria-tions spread light from a point source into a strip. The lenses are mounted in the examination eyeglasses in such a manner that the strips of light form a diagonal cross in patients with intact binocular vision. The patient is asked to describe the pattern of the strips of light while looking at the point source. Patients who describe a cross have normal simultaneous vision. Patient who see only one diagonal strip of light are suppressing the image received by the respective fellow eye.
Lang’s test:
This test may be used to determine depth perception in infants.
Acard depicts various objects that the child only sees if it can perceive
depth.
Related Topics