Chapter: Modern Medical Toxicology: Neurotoxic Poisons: Inebriants
Barbiturates - Inebriant Neurotoxic Poisons
Barbiturates
·
The barbiturates are derivatives of
barbituric acid (2,4,6-triox-ohexahydropyrimidine) and were extensively used as
sedative-hypnotics till the 1960s when the benzodiazepines arrived and quickly
displaced them.
Examples
·
Long acting (duration of action 6–12
hrs)
o Mephobarbitone
o Phenobarbitone.
·
Intermediate acting (duration of
action 3–6 hrs)
o Amobarbitone
o Aprobarbitone
o Butobarbitone.
·
Short acting (duration of action
< 3 hrs)
o Hexobarbitone
o Pentobarbitone
o Secobarbitone.
·
Ultra-short acting (duration of
action <15–20 min)
o Thiopentone
o Methohexitone.
Uses
·
Sedative-hypnotic.
·
Pre-operative sedation.
·
Treatment of seizure disorders.
Usual Fatal Dose
· Phenobarbitone: 6 to 10 grams.
· Amobarbitone, pentobarbitone,
secobarbitone: 2 to 3 grams.
·
Lethal blood level for short- and intermediate-acting barbi-
turates varies from 3 to 4 mg/100 ml, while for phenobar-bitone
it ranges from 8 to 15 mg/100 ml.
Toxicokinetics
·
Most barbiturates which are used as
sedative-hypnotics are administered orally. Intravenous route is usually
reserved for management of status epilepticus or induction/mainte- nance of
general anaesthesia.
·
Following absorption, barbiturates
are distributed widely.The long acting barbiturates have a plasma half-life of
about 80 hours.
·
Metabolism of most of these drugs
occurs by oxidation in the liver resulting in the formation of alcohols,
ketones, phenols, or carboxylic acids which are excreted in the urine as such
or in the form of glucuronic acid conjugates. Metabolism of barbiturates is
more rapid in children and is slower in the elderly.
Adverse Effects
·
Residual depression after the main
effect of the drug has passed off.
·
Paradoxical excitement (especially
in the elderly).
·
Hypersensitivity reaction—localised
swelling of eyelid, Synergistic action with ethanol and antihistamines.
·
cheek, or lip, erythematous or
exfoliative dermatitis.
·
Barbiturates are contraindicated in
patients with acute inter-mittent porphyria since they enhance porphyrin
synthesis.
Clinical (Toxic) Features
· Slurred speech, ataxia, lethargy,
confusion, headache, nystagmus. CNS depression, coma, shock.
· Pupils are at first constricted, but
later dilate because of hypoxia. Hypothermia.
· Cutaneous bullae (“barb burns”, barbiturate blisters):
These are clear, erythematous or haemorrhagic blisters, and occur in various
areas of the body, most typically on the hands, buttocks, and between the ankles
and knees, usually over pressure points. These lesions have also been reported
over non-pressure points, such as dorsal surfaces of fingers and toes, and
ocular conjunctiva.
· Death may occur from respiratory
arrest or cardiovascular collapse. Delayed death may be due to acute renal
failure, pneumonia, pulmonary oedema, or cerebral oedema.
· Chronic barbiturate (ab)use is
associated with the develop-ment of tolerance which is responsible for
decreasing the therapeutic to toxic index. An addict may obtain therapeutic
benefit only with 5 to 6 times the normal dose. Abrupt withdrawal results in
anorexia, tremor, insomnia, cramps, seizures, delirium, and orthostatic
hypotension.
Diagnosis
·
Serial plasma levels may be useful
in the management of phenobarbitone overdose. Plasma levels exceeding 8 mg/ dL
(80 mcg/mL) (344 mcmol/L) are generally associated with some degree of coma. In
the absence of tolerance, plasma levels exceeding 2 to 3 mg/dL may be
associated with CNS depression.
·
EEG: alpha coma* indicates poor prognosis.
Treatment
Monitor
CBC, serum electrolytes, glucose, blood urea nitrogen, creatinine, and urine
myoglobin in patients with significant intoxication. The onset of toxic effects
is usually within 2 hours, but peak toxicity may not occur for 18 or more
hours. All patients with a detectable phenobarbitone level require a repeat
serum phenobarbitone level at approximately 6 hours after the initial level. If
the repeat serum phenobarbitone level is within the therapeutic range, the
patient has been decontaminated, and is asymptomatic, the patient is not at
risk of toxicity. If the repeat serum phenobarbitone level is greater than the
initial level, additional levels are needed to follow the course of overdose.
·
Gastric lavage (preferably with a large-bore,
double-lumen tube),
can be done with benefit upto 12 to 24 hours post-ingestion.
·
Activated charcoal in the usual dose. Multiple dose
acti-vated charcoal has been shown to greatly increase pheno- barbitone
elimination in animal studies, volunteers, and overdose patients.
·
Forced alkaline diuresis is said to be particularly useful
in phenobarbitone poisoning. However, it should be considered only in severe
barbiturate toxicity with life-threatening signs and symptoms. It appears to be
less effective than multiple dose activated charcoal, and is generally not the
preferred method of elimination enhancement. Forced diuresis is of no value in
the treatment of short acting barbiturate intoxication.
·
Haemodialysis or haemoperfusion: Barbiturate elimination can
be increased by haemodialysis or charcoal haemop- erfusion. However, these
techniques are rarely needed when managing even severe barbiturate
intoxication, and should be reserved for patients with haemodynamic compromise
refractory to aggressive supportive care. Even though haemoperfusion can clear
barbiturates two to four times more rapidly than dialysis, haemoperfusion will
not correct electrolyte imbalances, and has been associated with platelet
consumption, hypothermia, hypotension, and decreased serum calcium.
·
Exchange transfusion may be beneficial in severe cases.
·
For hypotension: First administer 10 to 20 ml/kg of isotonic
intravenous fluids and place in Trendelenburg position. Repeat boluses of
isotonic intravenous fluids should be administered prior to initiating
vasopressor therapy. If the patient is unresponsive to isotonic fluid therapy
administer a vasopressor. Dopamine or noradrenaline should be titrated to
desired response.
·
Supportive measures: supplemental oxygen, intubation,
assisted ventilation, IV fluids.
·
Withdrawal may be treated by reinstitution of
phenobar-bitone, and a programme of gradual reduction over three weeks. A
tapering schedule of 10 percent every 3 days has been used successfully.
Autopsy Features
·
Peripheral cyanosis.
·
Froth at the mouth and nose.
·
Barbiturate
blisters on the dependant parts of skin surface*: buttocks, inner
aspects or back of thighs, calves, and fore- arms.
·
Intensely congested lungs.
·
Congestion or even erosion of the
stomach.
Forensic Issues
·
The incidence of poisoning with barbiturates has declined
dramatically in recent years as a direct result of decline in their use as
sedative-hypnotics. However cases do get reported even today, mostly the result
of deliberate self-ingestion. This type of (suicidal) poisoning was rampant in
the 1960s when these drugs were widely prescribed and consequently abused. One
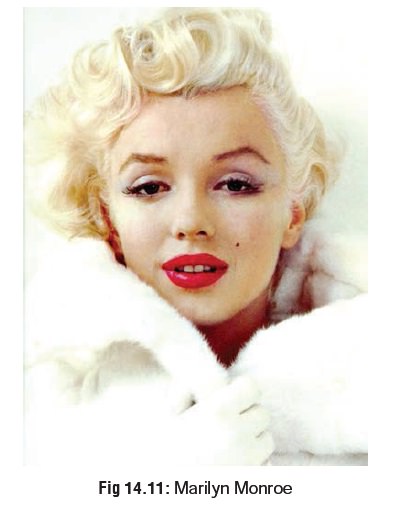
of the most famous cases during this period concerned immortal Hollywood
actress Marilyn Monroe (Fig 14.11) who at the end of her short,
tempestuous career became hopelessly addicted to alcohol and barbitu- rates. In
1962, at the age of 36, Marilyn Monroe was found dead at home following an
overdose of barbiturates.
·
In most parts of the world today, the few barbiturates still
used in therapeutics comprise phenobarbitone and thio- pentone. The latter
being available only as an injectable preparation has never been popular for
committing suicide. Nevertheless there have been reported cases.
·
In India, as per some studies, barbiturates used to account
for the maximum number of poison-related fatalities every year right upto the
early 1970s, but after that the incidence has plummeted rapidly, and today they
account for only a negligible proportion of deaths.
·
Accidental barbiturate poisoning due to inadvertent over-
dose is not uncommon among addicts because of their phenomenon of tolerance.
But earlier hypotheses that a patient could overdose himself to death by
so-called auto- matic behaviour brought
on by sleepy confusion have not withstood scientific analysis.
· Intravenous thiopentone has been used as truth serum to extract confessions during interrogation by inducing a state of drowsy disorientation in the course of which the person may reveal the truth. This controversial practice is closely related to the legitimate psychiatric practice of narcoanalysis used to diagnose certain mental ailments by placing the patient in a reclining position and administering amylobarbitone or some other short-acting barbiturate intra- venously until lateral nystagmus is induced or drowsiness is noted, when the interview is begun and sustained in a gentle fashion with periodic maintenance doses of the drug. This is sometimes referred to as the “Amytal interview”, Amytal being a popular trade name for amylobarbitone in some Western countries.
Related Topics