Chapter: Medicine Study Notes : Infectious Diseases
Bacterial Meningitis - Infections of the CNS
Infections of the CNS
Bacterial Meningitis
Signs and Symptoms
· Rapid onset of:
o Meningism: Headaches, photophobia, stiff neck. Kernig‟s sign: Pain on straightening knee with hip flexed
o ICP: Headache, irritable, drowsy, vomiting, fits, ¯pulse, ¯BP, ¯LOC, pin-point pupils, papilloedema (late sign), tense fontanelle
o Septicaemia: fever, arthritis, DIC, ¯BP, pulse,
tachycardia, rash (ultimately 80% will have a purpuric rash, 10 – 15% will have
a maculo-papular or urticarial rash, 5 – 10% will have no rash)
· In different age groups:
o Infants/toddlers: fever, lethargy, poor feeding, vomiting, toxic (drowsy, pallor), rash. Only 30 – 50% have signs of meningism Þ absence doesn‟t exclude. Bulging anterior fontanelle – but if vomiting may be normal or reduced
o Children > 3: fever, headache, vomiting, photophobia, stiff neck,
confusion (may be combative), non-blanching rash (initially blotchy macular
rash that rapidly becomes petechial or purpuric)
o Adolescents: may present as acute mania or appearance of drug induced
psychosis
Pathogenesis
· Organisms:
o Neonates: E. Coli, b-haemolytic streptococci Group B (eg streptococcus agalactiae – normal vaginal flora), rarely listeria
o Children < 14 years: H. Influenza (if < 4 and not immunised), Neisseria Meningitidia Type B, Strep Pneumoniae, Tb
o Adults: Neisseria Meningitidia Type B, Strep Pneumoniae, maybe staph
aureus or Cryptococcus neoformans
o Elderly, Immunocompromised: Pneumococcal, Listeria, Tb, G –ive,
Cryptococcus Neoformans
·
Pathogenesis:
o Pathology: inflammation of pia mater and arachnoid
o Most common are N Meningitidis and S pneumoniae
o Nasopharynx®blood®subarachnoid space (via choroid plexus): N meningitides, HIB, S. pneumoniae
o Middle ear®blood®subarachnoid space: S Pneumoniae, HIB
o Congential abnormalities (eg spina bifida): coliform bacilli,
pseudomonas, Strep agalactiae
o Trauma: Skull fracture + CSF leak, CNS surgery, shunts: Staph aureus
o Depressed immunity: listeria monocytogenes, cryptococcus neoformans
o Neonatal meningitis from vaginal flora (especially with prematurity,
prolonged ROM, delayed 2nd stage): Strep agalactiae, coliforms (E coli), listeria monocytogenes
·
If recurrent:
o Consider immunosuppression (eg hypogammaglobulinaemia or complement
deficiency)
o Look for lumbosacral defects, especially if enteric bacteria or S aureus
Investigations
·
Do blood culture before
presumptive treatment if possible, but NOTHING should delay presumptive
treatment. Tell lab about antibiotics
·
Must do:
o Blood cultures
o CSF via lumbar puncture unless contraindicated (see below)
o Urine: supra-pubic aspiration or catheter
o If antibiotics have already been administered:
§ Needle aspirate purpuric lesions for gram stain and culture
§ Throat swab
·
Bloods:
o Blood Glucose sample – may be hypoglycaemic [ABC = Airway, breathing,
circulation. DEFG =
o Don‟t Ever Forget Glucose]
o FBC, electrolytes, clotting time, ABGs
·
Lumbar puncture:
o Contraindicated if:
§ Signs of ICP (all meningitis will have ICP) causing cerebral herniation (eg very ¯LOC, very bad headache, focal signs including abnormal papillary reflexes, tonic seizures, decerebrate or decorticate posturing, irregular respirations, bradycardia, papilloedema). If in doubt then CT
§ Severe cardiovascular compromise with DIC/coagulopathy (eg fulminant
sepsis)
§ Infection over the injection site
o Tests of CSF: Gram stain, Tb, cytology, virology, glucose, protein,
India ink (Cryptococcus), culture (if clear then ?virus), antigen testing
(especially if partially treated)
o May be normal, repeat if symptoms persist
o Typical CSF (lots of variation):
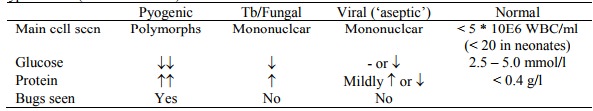
§ NB: early viral meningitis may have predominantly polymorphs
§ RBCs: None. If there are then either traumatic (more in 1st of 3 tubes) or bleed (new if
red, yellow if old – zathachromia)
o Appearance on Gram stain:
§ N Meningitidis: G –ive diplococci
§ H influenzae: Pleomorphic G –ive bacilli
§ S pneumoniae & S agalactiae: G +ive diplococci
§ Listeria: G +ive bacilli
§ TB: Acid fast bacilli very scant – take at least 5 mls of CSF
§ Cryptococcus neoformans: Indian ink stain shows capsules
·
Imaging: To identify subdural
collections, abscess, hydrocephalus, thrombosis and infarction. Only if LP
contraindicated and suspected mass lesion or persistent or focal neuro signs
Management
·
Management (based on protocol for
a child):
o Standard infection control precautions plus surgical mask when examining
throat, intubating etc
o ICU if:
§ Coma
§ Circulatory collapse
§ Persistent, recurrent seizures
§ SIADH with cerebral oedema or seizures
o Shock or ICP is what kills
o Maintain perfusion:
§ Colloid bolus (20 – 40 ml/kg 4% albumen iv), then colloid + glucose
§ Inotrope eg dobutamine (10 mg/kg/min)
§ Watch for ADH secretion ® hyponatraemia and cerebral oedema if too much fluid given
§ Check Na 6 – 12 hourly. If Na
< 135 mmol/l then ¯iv rate. If Na > 145 then rate
o Respiratory support:
§ O2
§ Early elective intubation if persistent shock (but may exacerbate hypotension due to vasodilation and ¯sympathetic drive)
§ Immediate intubation if ICP, hypoxia and/or respiratory failure, pulmonary oedema or hypotension (uncompensated shock)
o Correct abnormalities: anaemia, hypoglycaemia, coagulopathy (FFP), acidosis
(NaHCO3), hypokalaemia
o Seizures: anticonvulsants
o Watch for ICP:
§ ¯Conscious
state, focal neuro signs, abnormal pupils, hypertension and relative
bradycardia.
§ Treatment: ICU, ¯PCO2, diuretics (Mannitol, frusemide), head up, deep sedation, inotropes. But priority is to correct the shock (CBF = MAP – ICP)
o Weight and measure head daily in an infant
o Isolate patient, ensure analgesia
o Dexamethasone treatment controversial (most benefit in HIB). Not
routinely used. Reduces fever and gives misleading impression of clinical
improvement
· Antibiotic regimes:
o Empiric antibiotic treatment:
§ Neonate – 3 mths: Amoxycillin 50 mg/kg (for listeria) + Ceftriaxone 50
mg/kg (E coli and Strep). 2 weeks for G +ive, 3 weeks for G –ive.
§ Older child:
·
Cefotaxime 50 mg/kg/6hr, max 2 g,
iv for 7 – 10 days or
·
Ceftriaxone 50 mg/kg/12hr, max 2
g, iv for 7 – 10 days or
· Penicillin G 50 mg/kg/4hr iv for 7 – 10 days
§ If strep pneumonia suspected: Vancomycin 15 mg/kg/6hr, max 500 mg, iv + cefotaxime/ceftriaxone – synergistic, necessary due to resistance to 3rd generation cephalosporins
§ If still failing consider adding Rifampicin
o Specific Treatment according to culture and susceptibility results:
§ N Meningitidis, S agalactiae: Penicillin (Cefotaxime if allergic to
penicillin) for 5-7 days. For meningococcaemia only can use penicillin or
cefotaxime
§ S pneumonia:
·
Penicillin susceptible:
penicillin (but 20% are resistant) for 7 – 10 days
·
Penicillin resistant, 3rd generation susceptible:
Cefotaxime
·
Penicillin and 3rd generation resistant: Cefotaxime
+ Vancomycin
§ H Influenza: Cefotaxime, Ceftriaxone
§ L Monocytogenes: amoxycillin
§ Staph Aureus: Flucloxacillin
§ M Tuberculosis: Rifampicin, Isoniazid, Pyrazinamide, Ethambutol
§ Coliforms: 3rd generation Cephalosporin (ie Cefotaxime, Ceftazidime)
§ Pseudomonas: Ceftazidime
§ Cryptococcus Neoformans: fluconazole or amphotericin B
§ NB: Erythromycin and gentamycin don‟t have good CSF penetration
o If not responding, or non-susceptible strain of pneumococci or receiving dexamethasone than repeat LP after 24 – 48 hours
·
Complications:
o Seizures:
§ First suspicion should be hyponatraemia (also hypoglycaemia):
·
SIADH (Na < 130 and urine Na
> 20) ® exacerbates cerebral oedema
· Prevent by restricting fluids to 50% of maintenance
· Treatment: severe fluid restriction (10 ml/kg/day), in an emergency consider hypertonic saline, Mannitol or frusemide
§ Hypoventilation can further ICP ® hypoxia,
hypercapnea, acidosis
§ Anticonvulsants can also exacerbate these metabolic changes
§ Management options: diazepam, clonazepam, phenobarbitone, dextrose to control hypoglycaemia, intubation and ventilation
o Major disability in 15%: Deafness,
brain damage, peripheral necrosis, etc. All cases should have audiologist check
within 6 – 8 weeks of discharge
o Death in 5%, 10 –15% pneumococcal meningitis, 20% in fulminant
meningococcaemia
Meningococcal Disease
·
Cause: Neisseria Meningitidia
· Epidemiology:
o 10-year epidemic started in 1990 with about 50 reported cases. Since
then 3696 cases and 163 deaths. Current case fatality rate is 3 – 5 %
o Leading infectious cause of death in children
o 500 reported cases in 2000. NZ
rate is 13.3 per 100,000. UK rate is 4 per 100,000
o Regional variation: East Cape and Central North Island the highest
o Rates per 100,000 < 1 year olds:
§ Pacific Island: 570
§ Maori: 230
§ European: 80
·
Healthy people can be carriers
·
Transfer via respiratory
secretions
·
Kids and teenagers more
susceptible than adults
· Not a cause of Otitis media
·
Pathogenesis: endotoxins
(lipopolysaccharides in the cell wall) activate complement and release of PAF
causing endothelial injury ® immune activation and vascular permeability
· Notifiable to public health (as is HIB)
· Prophylaxis to stop nasal carriage of the bug – not to cure incubating illness. Nasal carriage higher in adults than children
o Rifampicin: 4 doses, 600 mg bd for adults, 10 mg/kg bd for kids (very high dose). Broad spectrum antibiotic
o Offer to index case (if only treated with penicillin), all intimate,
household and day-care contacts during last 10 days
o Contraindications: pregnancy (use single dose ceftriaxone), liver disease.
o Side effects: nausea, vomiting, diarrhoea (GI effects), turns urine/tears/sweat orange/red (will stain contacts)
o Interactions: asthma, blood clotting and oral contraceptives (continue
pill, use barrier method until 7 days after antibiotics finished)
TB Meningitis
·
Rare
·
Most common < 5 years
·
Slow onset: malaise and fever
progressing to drowsiness, neck stiffness and seizures over 2 weeks
·
Mantoux testing may be normal,
and CXR normal in ½ of cases
·
Investigations:
o Gastric lavage, urine and CSF for Acid fast stain and culture
o CT
·
Treatment: isoniazid, rifampicin,
pyrazinamide
·
Notifiable disease
Related Topics