Chapter: Clinical Cases in Anesthesia : Blood Replacement
Who is eligible and what are the contraindications for PABD?
Who is eligible and what are the contraindications for PABD?
PABD is limited to cases where there is a
reasonable like-lihood that red cell transfusion will be required during the
perioperative period. A surgical blood loss of 1,000 mL or more should be
anticipated. The surgical blood schedule serves as a guide to whether or not
transfusion is likely. Patients should not be encouraged to donate blood for
procedures in which there is little chance of significant blood loss.
Criteria for donation of autologous blood are
less strin-gent than those for volunteer donation. Autologous donors need a
predonation Hb of 11 g/dL or higher or Hct of 33% or higher. Age is not a
criterion for predonation, which has been used in the elderly and the pediatric
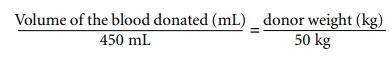
populations. In patients weighing more than 50 kg, 450 mL of whole blood are
donated at each visit. In patients weighing less than 50 kg, the volume of
blood removed is proportional to weight, using the formula:
PABD requires a suitable interval between the
decision to undertake surgery and the actual date of the operation. The storage
life of blood is 35 days. Consequently, there is no point in donating blood
more than 5 weeks preopera-tively. A unit of blood may be banked every 3 days
depend-ing on the donor’s Hct, but donations are usually made every 7 days.
Units can be stored for up to 3 days preoper-atively. In the event that surgery
is postponed blood may be frozen to prevent outdating if necessary.
In rare cases where collection of large numbers
of autol-ogous units is required, blood may be frozen and stored over long
periods of time. Patients should be started on oral iron therapy once the
decision to predonate blood is made. Use of recombinant erythropoietin to
increase the amount of blood available for predonation and to decrease the interval
between donations has been described and may be beneficial in patients who are
anemic, who require large numbers of autologous units, or where the
presurgi-cal intervals are short. Erythropoietin therapy as described is
expensive and remains experimental as of this writing.
There are several contraindications to PABD.
Because bacteria may proliferate during blood storage, bacteremia is an
absolute contraindication to predonation. Lack of intravenous access may also
prohibit predonation.
Patients who are positive for HIV or hepatitis
B surface antigen (HBsAg) may predonate blood. Such units must be
labeled and segregated to protect other patients who might erroneously receive
the unit, as well as workers handling it. Retransfusing this blood requires a
special order from the patient’s physician.
As in other aspects of transfusion medicine,
patients with cardiac disease represent a gray area in terms of risk. Most
centers exclude patients with unstable angina, aortic stenosis, or left main
coronary artery disease but will accept donors with stable coronary artery
disease. Some investigators have advocated monitoring (blood pressure,
electrocardiograph, pulse, and oxygen saturation), simultaneous fluid
adminis-tration, and physician supervision of high-risk patients making
autologous donations. Precise delineation of risk in these patients awaits the
outcome of future studies.
In contrast to homologous blood donation, a
history of malignancy does not contraindicate PABD.
Related Topics