Chapter: Clinical Cases in Anesthesia : Blood Replacement
Explain the advantages and disadvantages of different autologous blood sources
Explain the advantages and disadvantages of different autologous
blood sources.
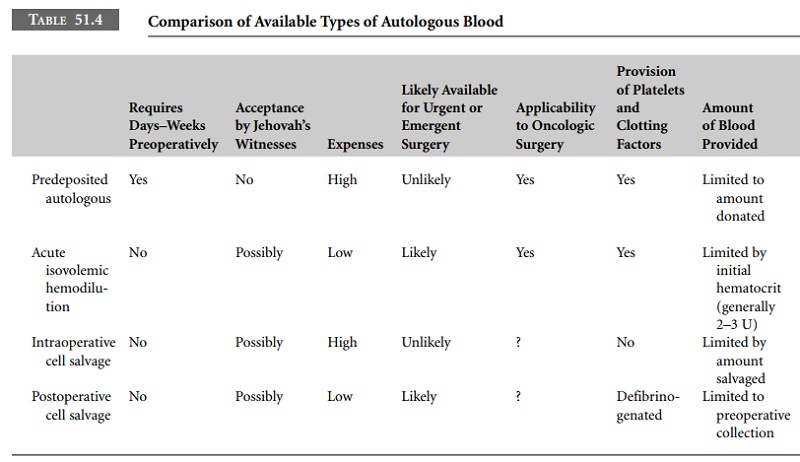
Much controversy, and little consensus, exists
in the lit-erature about the “best” way to utilize autologous blood, with some
experts advocating one method and others another. If it is not clear which
method is superior, it is clear that each has something to offer, with the
relative strengths and weaknesses of each method dependent on the clinical
circumstances (Table 51.4).
PABD has the disadvantages of being relatively
expen-sive, subjecting patients to some of the same risks as homologous
transfusion (administrative error, storage lesion), and requiring a substantial
time interval between harvesting the blood and the date of surgery. If blood is
donated too close to the date of surgery, with insufficient time for the
resynthesis of red cells to compensate for the amount removed, patients can be
relatively anemic at the time of surgery and tend to leave the hospital with a
lower Hct compared with controls. However, if blood is collected at a suitable
interval before surgery, so that substantive erythropoiesis can occur, PABD can
be a highly effective method of preventing exposure to homologous blood. A
survey of 1,000 hospitals recently found that PABD is the most commonly
practiced method of blood conservation. Its use is widely accepted by patients,
and in some states in the United States (California), discussion of PABD is
mandatory as part of informed consent for any operation in which blood
transfusion is likely.
AIHD has the advantage of being inexpensive,
and is a “point-of-care” intervention. It obviates the need for
weeks-in-advance planning and eliminates the risk of administra-tive error
associated with stored blood. A number of clinical studies purport to show that
it is of comparable efficiency, with less cost, to PABD or cell salvage.
However, other stud-ies, as well as mathematical models, have shown that the
amount of red blood cells saved by AIHD is quite small and usually clinically
insignificant. For AIHD to be clinically useful, both low Hct and large
surgical blood losses must be safely tolerated. A number of authors have raised
concerns about the iatrogenic introduction of risk in patients with previously
unappreciated cardiac disease from moderate or profound hemodilution. Because
of such concerns, the use of AIHD is probably of limited benefit to older
patients. Its use is probably least contro-versial, and of greatest benefit, in
pediatric or young adult patients with a low likelihood of unappreciated
cardiac disease, who are not anemic, and who are having surgeries with large
anticipated blood loss.
Intraoperative cell salvage is a widely used
and highly effective method of reducing patients’ exposure to homol-ogous
blood, and in cases involving large amounts of bleeding this procedure can
rapidly provide autologous blood for return. Its use has been criticized
largely on the grounds of cost-effectiveness, with the “break-even” point being
2 units of blood. However, by initially setting up only the collection
(suction) part of the apparatus, and setting up the remainder, and more costly
portion, of the machine only if a sufficient amount of blood has been
collected, unnecessary costs associated with cell salvage can be decreased.
Though there has been theoretical concern about the use of cell salvage in
cases involving possible contamination of the blood with malignant cells or
bacteria, clinical studies and experience have not shown an increase in either
metastatic tumor spread or infection rates. Intraoperative cell salvage is an
essential part of blood conservation programs.
Scientific advances over the past decade have
greatly decreased the likelihood of transmission of viral diseases such as HIV
and hepatitis C via blood transfusion. Nonetheless, avoidance of blood
transfusion remains a significant concern on the part of the public, and has
been identified as one of the most important factors in a patient’s decision as
to where to seek medical care. Furthermore, the potential impact of emerging
diseases as West Nile virus, severe acute respiratory syndrome (SARS), and
spongiform encephalopathies on the safety of the blood supply is of concern to
both the public and the medical community. Spurred by such factors, the
popularity of so-called bloodless surgery programs, designed to reduce or
minimize exposure to homologous blood, has increased, and such programs are
offered by approximately 100 centers in the United States.
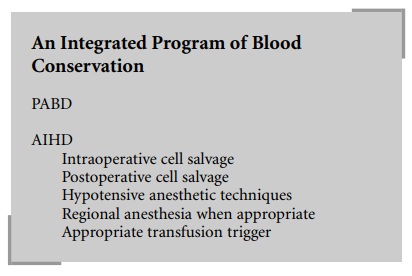
A comprehensive program to decrease homologous
blood exposure utilizes all of the techniques discussed in this chapter.
Additional factors in attempting to decrease blood loss include careful
surgical techniques, maintenance of normothermia, use of regional anesthesia,
and in select patients, use of hypotensive general anesthesia. When combined
with the use of an appropriate transfusion trig-ger, these techniques all
contribute to minimizing patient exposure to homologous blood.
Related Topics