Chapter: Clinical Cases in Anesthesia : Blood Replacement
Outline the disadvantages and risks of PABD
Outline the disadvantages and risks of PABD.
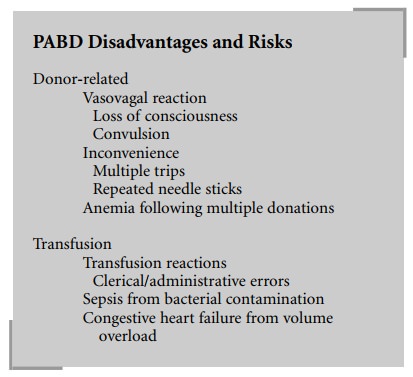
First, it should be noted that some of the risks associated with blood transfusions - ABO incompatibility due to clinical/administrative error and bacterial contamination - are not eliminated by use of PABD. For this reason, it is generally argued that the criteria for transfusing a unit of autologous blood (i.e., transfusion trigger) should be the same as for a unit of homologous origin. Others argue that, as the risks associated with autologous blood are decreased relative to homologous blood, then the risk/benefit ratio is altered, and the criteria for transfusion of autologous blood should be liberalized.
Paradoxically, use of PABD can result in a
lower Hct, on average, of discharged patients. This is because many patients who
predonate blood do not have adequate time, in the interval before surgery, to
fully regenerate the amount of blood they have donated. Thus, they are
essen-tially hemodiluted at the time of surgery. If they do not then receive a
blood transfusion (because of low intraoper-ative blood loss), their discharge
Hct will be lower then if they had not predonated.
Similarly, in an era of cost-effectiveness
analysis, the use of PABD has been challenged. In certain surgical settings
(i.e., total joint replacement), the use of PABD decreases by approximately 70%
the likelihood that a patient will require homologous transfusion. In other
settings (i.e., hysterectomy), many fewer patients will require transfusion,
and a higher percentage of the units collected by PABD are discarded. Factors
that increase the cost-effectiveness of PABD include appropriate case selection
(cases where there is a high likelihood that the units will be transfused) and
providing a long enough time interval between donation and surgery to allow
regenerative erythropoiesis to occur. The use of erythropoietin therapy in
conjunction with PABD makes logical sense and is being investigated.
From the patient’s standpoint, multiple trips
to the hospital or blood center to donate blood are inconvenient, and repeated
needle sticks are uncomfortable. Vasovagal reactions occur in 2–5% of patients,
of whom 0.3% will lose consciousness and 0.03% will convulse. In one study,
1:16,783 autologous donations led to an adverse event requiring
hospitalization, a rate higher than that reported in normal volunteers.
Blood collected for autologous use is subjected
to the same tests as homologous blood. If not used, it is not “crossed over”
into the general blood pool, but is discarded, as it is not felt that patients
donating blood for autologous use are truly volunteer donors.
Related Topics