Chapter: Medicine and surgery: Cardiovascular system
Ventricular septal defects - congenital heart disease
Ventricular septal defects
Definition
Abnormal defect in the ventricular septum allowing passage of blood flow between the ventricles.
Incidence
1 in 500 live births, the commonest of all heart defects accounting for around 40%.
Age
Congenital
Sex
M = F
Aetiology
In most cases the aetiology is unknown but may include maternal alcohol abuse. In Down syndrome the combination of atrial and ventricular septal defects may lead to formation of a complete atrioventricular defect with a single AV valve. In other patients ventricular septal defects may also occur in combination with other defects as a part of a complex congenital heart disorder.
Pathophysiology
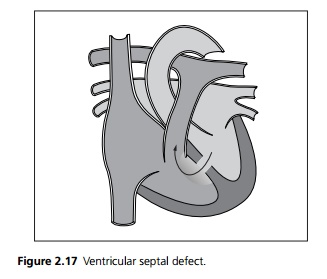
Most ventricular septal defects occur in the membranous part of the ventricular septum, although muscular defects do occur (see Fig. 2.17).
┬Ę Small defects result in little blood crossing to the right side of the heart and no haemodynamic compromise ŌĆō ŌĆśmaladie de RogerŌĆÖ. The murmur is loud as there is a small jet of turbulent flow across the defect.
┬Ę Large defects with low pulmonary vascular resistance result in a large left to right shunt of blood with volume overload in the left ventricle. The murmur is, however, quieter as there is less turbulent flow.
Initially increased pulmonary blood flow does not cause a rise in pressures within the pulmonary circulation due to the vascular compliance. If, however, there is a continued large left to right shunt, the combination of increased pulmonary blood volume and high-pressure shear forces causes hypertrophy and deposition of collagen in the walls of pulmonary arterioles. Eventually these changes become irreversible and pulmonary hypertension develops, usually during childhood. The resultant high pressure in the right side of the heart causes a reduction and eventual reversal of the shunt with associated development of cyanosis termed Eisenmenger syndrome.
Clinical features
VSDs cause a variety of presentations depending on the size of the defect.
┬Ę Small defects presents with an asymptomatic loud pansystolic murmur heard loudest at the left sternal edge due to flow across the defect, there may be an associated thrill.
┬Ę Large left to right shunts may cause cardiac failure, which may not develop until late childhood. On examination there is usually a pulmonary ejection murmur and there may be tachypnoea and tachycardia if cardiac failure is present.
┬Ę Large defects with pulmonary hypertension and hence right to left shunts cause cyanosis. There may be a parasternal heave. The high right heart pressures causes a loud pulmonary component to the second heart sound.
Investigations
┬Ę Chest X-ray: Abnormalities are only seen with large defects when cardiomegaly and prominent pulmonary vasculature may be seen.
┬Ę ECG is normal in small defects, evidence of left and right ventricular hypertrophy may be seen in larger defects.
┬Ę Echocardiography is diagnostic. Measurement of the size of the defect and the blood flow allows prediction of the outcome.
Management
┬Ę Prophylaxis against infective endocarditis is advised. If cardiac failure is present it should be treated appropriately.
┬Ę Small defects usually close spontaneously, large defects with significant left to right shunts require surgery often before school age to prevent Eisenmenger syndrome. The defect is closed, often using a Dacron patch, under cardiopulmonary bypass.
┬Ę If the pulmonary hypertension has developed and the shunt direction has reversed, surgery is contraindicated. Heart and lung transplant may be considered.
Prognosis
Up to 50% may close spontaneously usually in early childhood, the hole may remain the same size (the heart grows so the defect becomes comparatively smaller).
Related Topics