Chapter: Medicine and surgery: Cardiovascular system
Chronic stable angina - Ischaemic heart disease
Chronic stable angina
Definition
Chest pain occurring during periods of increased myocardial work because of reduced coronary perfusion.
Incidence
Angina is common reflecting the incidence of ischaemic heart disease.
Age
Incidence increases with age.
Sex
M > F. Premenopausal women are relatively protected.
Geography
Predominantly a disease of the Western world, but this pattern is changing with the increasing affluence of the developing world.
Aetiology
Angina is most commonly associated with atheroma, although exertional chest pain can occur with other conditions, such as aortic stenosis and hypertrophic cardiomyopathy. In ŌĆśstable anginaŌĆÖ, pain is precipitated by physical exertion, meals, cold weather and high emotion (anger, excitement), and it is relieved by rest.
Pathophysiology
The pathology of stable angina is the presence of high-grade stenosis of at least one coronary artery resulting in a reduction of at least 50% of the lumen diameter or 75% of the lumen area. The underlying mechanism is atheroma, which affects large and mediumsized arteries. The true pathogenesis of atheroma is not fully understood but the following factors are thought to play role:
Stage I: Damage to the endothelium of the arteries allows the entry of cholesterol rich LDLs into the intima. At this stage the cholesterol is extracellular.
Stage II: Normally macrophages are unable to phagocytose cholesterol as they lack the required receptor; however, once the LDLs are oxidised they are taken up by macrophages by a receptor-independent pathway. The resultant lipid-laden macrophages are termed foam cells, an accumulation of which causes a visible pale bulge called a fatty streak.
Fatty streaks are often visible within the first year of life, and these occur worldwide, even in areas where atheroma is uncommon. This suggests that the initiation of fatty streak may not be due to the risk factors for atherosclerosis.
Stage III: The macrophages release lipid and cytokines into the intima, resulting in the stimulation of intimal cell proliferation. These cells secrete collagen and the plaque becomes fibrotic. The result is a raised yellow lipid plaque.
Stage IV: The secreted collagen forms a dense fibrous cap. The lesion, now termed a fibrolipid plaque, contains free lipid as well as foam cells with an overlying fragile endothelium.
Clinical features
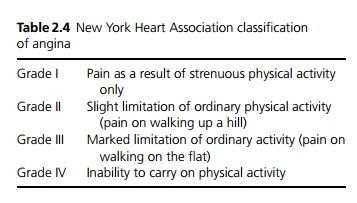
The classical description of angina pectoris is of a heavy chest pain, often described as like a tight band around the chest. It may range from a mild dull ache or mild chest tightness to a crushing, severe pain. It may radiate to the jaw or arms (especially the left), sometimes it is only in the jaw, neck, arm or hand. The nature of pain and its severity do not necessarily indicate the severity of disease. The pattern of pain is often more consistent. It is brought on by exertion or emotion and relieved within a few minutes of rest. A grading system exists based on the level of activity provoking pain (see Table 2.4). It is important to elicit whether there has recently been a reduction in the exercise tolerance (crescendo angina), or angina at rest.
Macroscopy
Atheroma tends to affect large and medium-sized arteries and is confined to the systemic circulation. There are
four patterns of plaque depending on its position and the ratio of the lipid pool to the fibrous cap: Concentric fibrous: 48% of plaques
Eccentric fibrous: 12% of plaques Concentric lipid rich: 28% of plaques Eccentric lipid rich: 12% of plaques
The eccentric lipid rich plaques are the most likely to ulcerate due to the markedly abnormal flow pattern through the vessel and the relatively thin fibrous cap.
Microscopy
Plaques are located in the intima of the arterial wall. They consist of a pale lipid rich area and a pink stained fibrous cap. They contain varying amounts of free lipid, collagen and foam cells. Late in the evolution of a plaque the underlying media becomes thinned by pressure atrophy.
Investigations
┬Ę The ECG is often normal, although there may be signs of hypertrophy and old infarction.
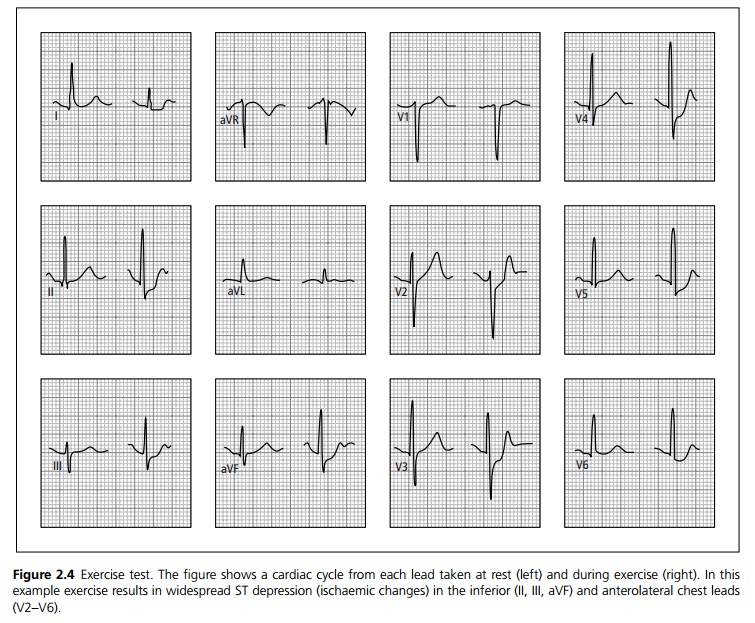
┬Ę Exercise ECG can determine exercise tolerance and usually shows ST depression or T wave changes in the distribution of the lesion (see Fig. 2.4).
┬Ę Thallium-201 uptake scan may show areas of infarction and reversible ischaemia.
┬Ę Echocardiogram both during resting and under stress (dobutamine) may show abnormal ventricular wall function.
┬Ę Coronary angiography can be used but carries a small morbidity and mortality risk.
┬Ę MRI angiography is non-invasive and may prove a useful alternative.
Management
Acute attack: stop exercise, use glyceryl trinitrate (GTN) sublingually.
General management includes identification and treatment of any exacerbating cause such as anaemia or thyrotoxicosis. Risk factor modification is crucial, in particular stopping smoking, treatment of hypertension, improving diabetic control and lowering cholesterol.
Medical management: aspirin or other antiplatelet agents such as clopidogrel reduce the risk of myocardial infarction. HMGCoA reductase inhibitors (statins), which lower cholesterol, are effective for primary and secondary prevention of myocardial infarction.
Symptomatic treatment may involve one or a combination of the following:
┬Ę ╬▓-blockers reduce the oxygen demand of the heart by reducing the heart rate and the force of ventricular contraction. They are particularly useful after a my-ocardial infarction to reduce the risk of a subsequent cardiac event.
┬Ę Long acting nitrates (oral or transcutaneous) are coronary artery dilators and are useful in patients who respond to sublingual GTN.
┬Ę Calcium channel blockers such as diltiazem and amlodipine reduce coronary artery tone. Diltiazem and verapamil also reduce the heart rate and the force of ventricular contraction resulting in a decreased myocardial oxygen demand. They should be used with care in conjunction with ╬▓-blockers or in patients with heart failure.
┬Ę Potassium channel openers such as nicorandil are third line agents.
If symptoms cannot be controlled by medication, the main choices for coronary intervention are between coronary angioplasty and coronary artery bypass surgery.
┬Ę Coronary artery bypass grafting is indicated where it may improve prognosis or when symptoms persist to an extent that interferes with normal life despite medical treatment. In patients with triple vessel disease or left main stem coronary artery disease, surgery impproves outcome. Operative mortality depends on several factors including age and concomitant disease.
┬Ę Percutaneous transluminal coronary angioplasty (PTCA) is carried out under local anaesthetic. A balloon is inflated in the coronary artery to reduce the stenosis.
Prognosis
Prognosis is dependent on severity of disease, number of coronary arteries affected, left ventricular function and coexistent disease such as diabetes mellitus, peripheral vascular disease, hypertension and renal impairment.
Related Topics