Chapter: Medical Physiology: Cardiac Arrhythmias and Their Electrocardiographic Interpretation
Ventricular Fibrillation
Ventricular Fibrillation
The most serious of all cardiac arrhythmias is ventricu-lar fibrillation, which, if not stopped within 1 to 3minutes, is almost invariably fatal. Ventricular fibrilla-tion results from cardiac impulses that have gone berserk within the ventricular muscle mass, stimulating first one portion of the ventricular muscle, then another portion, then another, and eventually feeding back onto itself to re-excite the same ventricular muscle over and over—never stopping. When this happens, many small portions of the ventricular muscle will be contracting at th
Phenomenon of Re-entry—“Circus Movements” as the Basis for Ventricular Fibrillation
When the normal cardiac impulse in the normal heart has traveled through the extent of the ventricles, it has no place to go because all the ventricular muscle is refractory and cannot conduct the impulse farther. Therefore, that impulse dies, and the heart awaits a new action potential to begin in the atrial sinus node.
Under some circumstances, however, this normal sequence of events does not occur. Therefore, let us explain more fully the background conditions that can initiate re-entry and lead to “circus movements,” which in turn cause ventricular fibrillation.
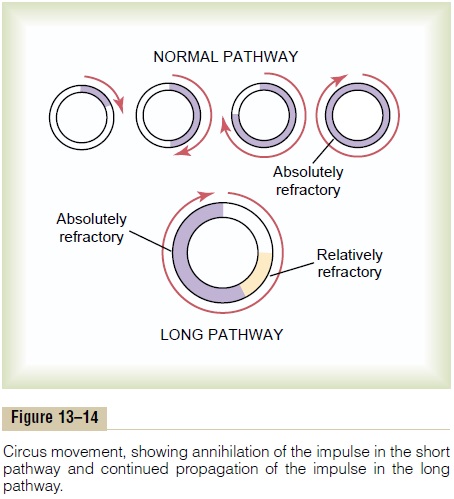
Figure 13–14 shows several small cardiac muscle strips cut in the form of circles. If such a strip is stimu-lated at the 12 o’clock position so that the impulse travelsin only one direction, the impulse spreads progressivelyaround the circle until it returns to the 12 o’clock posi-tion. If the originally stimulated muscle fibers are still in a refractory state, the impulse then dies out because refractory muscle cannot transmit a second impulse. But there are three different conditions that can cause this impulse to continue to travel around the circle, that is, to cause “re-entry” of the impulse into muscle that has already been excited. This is called a “circus movement.”
First, if the pathway around the circle is too long, by the time the impulse returns to the 12 o’clock position, the originally stimulated muscle will no longer be refractory and the impulse will continue around the circle again and again.
Second, if the length of the pathway remains constant but the velocity of conduction becomes decreased enough, an increased interval of time will elapse before the impulse returns to the 12 o’clock position. By this time, the originally stimulated muscle might be out of the refractory state, and the impulse can continue around the circle again and again.
Third, the refractory period of the muscle mightbecome greatly shortened. In this case, the impulse couldalso continue around and around the circle.
All these conditions occur in different pathological states of the human heart, as follows: (1) A long pathway typically occurs in dilated hearts. (2) Decreased rate of conduction frequently results from (a) blockage of the Purkinje system, (b) ischemia of the muscle, (c) high blood potassium levels, or (d) many other factors. (3) A shortened refractory period commonly occurs in response to various drugs, such as epinephrine, or after repetitive electrical stimulation. Thus, in many cardiac disturbances, re-entry can cause abnormal patterns of cardiac contraction or abnormal cardiac rhythms that ignore the pace-setting effects of the sinus node.
Chain Reaction Mechanism of Fibrillation
In ventricular fibrillation, one sees many separate and small contractile waves spreading at the same time in different directions over the cardiac muscle. The re-entrant impulses in fibrillation are not simply a single impulse moving in a circle, as shown in Figure 13–14. Instead, they have degenerated into a series of multiple wave fronts that have the appearance of a “chain reac-tion.” One of the best ways to explain this process in fibrillation is to describe the initiation of fibrillation by electric shock caused by 60-cycle alternating electric current.
Fibrillation Caused by 60-Cycle Alternating Current. At acentral point in the ventricles of heart A in Figure 13–15, a 60-cycle electrical stimulus is applied through a stimulating electrode. The first cycle of the electrical stimulus causes a depolarization wave to spread in all directions, leaving all the muscle beneath the electrode in a refractory state. After about 0.25 second, part of this muscle begins to come out of the refractory state. Some portions come out of refractoriness before other portions.
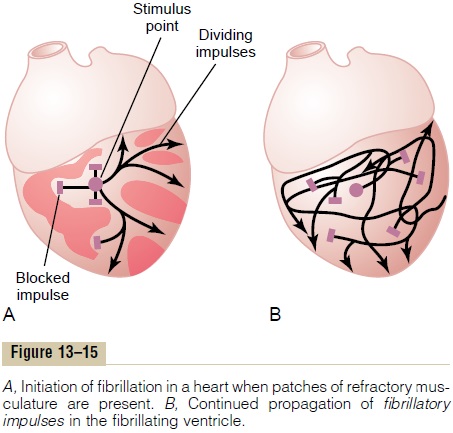
This state of events is depicted in heart A by many lighter patches, which represent excitable cardiac muscle, and dark patches, which represent still refrac-tory muscle. Now, continuing 60-cycle stimuli from the electrode can cause impulses to travel only in certain directions through the heart but not in all directions. Thus, in heart A, certain impulses travel for short dis-tances, until they reach refractory areas of the heart, and then are blocked. But other impulses pass between the refractory areas and continue to travel in the excitable areas. Then, several events transpire in rapid succession, all occurring simultaneously and eventuating in a state of fibrillation.
First, block of the impulses in some directions but suc-cessful transmission in other directions creates one of the necessary conditions for a re-entrant signal to develop—that is, transmission of some of the depolar-ization waves around the heart in only some directions but not other directions.
Second, the rapid stimulation of the heart causes two changes in the cardiac muscle itself, both of which pre-dispose to circus movement: (1) The velocity of conduc-tion through the heart muscle decreases, which allows alonger time interval for the impulses to travel around the heart. (2) The refractory period of the muscle isshortened, allowing re-entry of the impulse into previ-ously excited heart muscle within a much shorter time than normally.
Third, one of the most important features of fibrilla-tion is the division of impulses, as demonstrated in heart A. When a depolarization wave reaches a refractory area in the heart, it travels to both sides around the refractory area. Thus, a single impulse becomes two impulses. Then, when each of these reaches another refractory area, it, too, divides to form two more impulses. In this way, many new wave fronts are contin-ually being formed in the heart by progressivechainreactions until, finally, there are many small depolariza-tion waves traveling in many directions at the same time. Furthermore, this irregular pattern of impulse travel causes many circuitous routes for the impulses totravel, greatly lengthening the conductive pathway, which is one of the conditions that sustains the fibrillation. Italso results in a continual irregular pattern of patchy refractory areas in the heart.
One can readily see when a vicious circle has been initiated: More and more impulses are formed; these cause more and more patches of refractory muscle, and the refractory patches cause more and more division of the impulses.Therefore, any time a single area of cardiac muscle comes out of refractoriness, an impulse is close at hand to re-enter the area.
Heart B in Figure 13–15 demonstrates the final state that develops in fibrillation. Here one can see many impulses traveling in all directions, some dividing and increasing the number of impulses, whereas others are blocked by refractory areas. In fact, a single electric shock during this vulnerable period frequently can lead to an odd pattern of impulses spreading multidirection-ally around refractory areas of muscle, which will lead to fibrillation.
Electrocardiogram in Ventricular Fibrillation
In ventricular fibrillation, the electrocardiogram is bizarre (Figure 13–16) and ordinarily shows no ten- dency toward a regular rhythm of any type. During the first few seconds of ventricular fibrillation, relatively large masses of muscle contract simultaneously, and this causes coarse, irregular waves in the electrocardiogram. After another few seconds, the coarse contractions of the ventricles disappear, and the electrocardiogram changes into a new pattern of low-voltage, very irregu-lar waves. Thus, no repetitive electrocardiographic pat-tern can be ascribed to ventricular fibrillation. Instead, the ventricular muscle contracts at as many as 30 to 50 small patches of muscle at a time, and electrocardio-graphic potentials change constantly and spasmodically because the electrical currents in the heart flow first in one direction and then in another and seldom repeat any specific cycle.
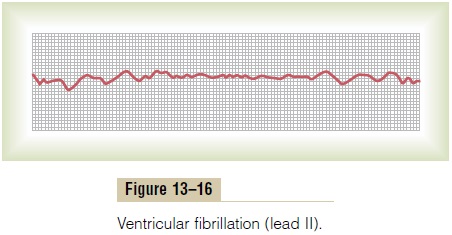
The voltages of the waves in the electrocardiogram in ventricular fibrillation are usually about 0.5 millivolt when ventricular fibrillation first begins, but they decay rapidly so that after 20 to 30 seconds, they are usually only 0.2 to 0.3 millivolt. Minute voltages of 0.1 millivolt or less may be recorded for 10 minutes or longer after ventricular fibrillation begins. As already pointed out, because no pumping of blood occurs during ventricular fibrillation, this state is lethal unless stopped by some heroic therapy, such as immediate electroshock through the heart.
Electroshock Defibrillation of the Ventricles
Although a moderate alternating-current voltage applied directly to the ventricles almost invariably throws the ventricles into fibrillation, a strong high-voltage alternating electrical current passed through the ventricles for a fraction of a second can stop fibrillation by throwing all the ventricular muscle into refractori-ness simultaneously. This is accomplished by passing intense current through large electrodes placed on two sides of the heart. The current penetrates most of the fibers of the ventricles at the same time, thus stimulat-ing essentially all parts of the ventricles simultaneously and causing them all to become refractory. All action potentials stop, and the heart remains quiescent for 3 to 5 seconds, after which it begins to beat again, usually with the sinus node or some other part of the heart becoming the pacemaker. However, the same re-entrant focus that had originally thrown the ventricles into fib-rillation often is still present, in which case fibrillation may begin again immediately.
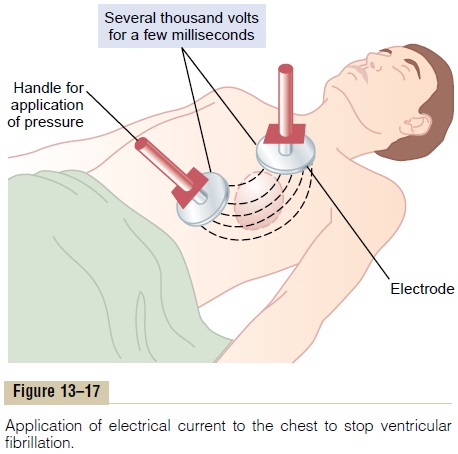
When electrodes are applied directly to the two sides of the heart, fibrillation can usually be stopped using 110 volts of 60-cycle alternating current applied for 0.1 second or 1000 volts of direct current applied for a few thousandths of a second. When applied through two electrodes on the chest wall, as shown in Figure 13–17, the usual procedure is to charge a large electrical capacitor up to several thousand volts and then to cause the capacitor to discharge for a few thousandths of a second through the electrodes and through the heart. In our laboratory, the heart of a single anesthetized dog was defibrillated 130 times through the chest wall, and the animal lived thereafter in perfectly normal condition.
Hand Pumping of the Heart (Cardiopulmonary Resuscitation) as an Aid to Defibrillation
Unless defibrillated within 1 minute after fibrillation begins, the heart is usually too weak to be revived by defibrillation because of the lack of nutrition from coro-nary blood flow. However, it is still possible to revive the heart by preliminarily pumping the heart by hand (intermittent hand squeezing) and then defibrillating the heart later. In this way, small quantities of blood are delivered into the aorta and a renewed coronary blood supply develops. Then, after a few minutes of hand pumping, electrical defibrillation often becomes possi-ble. Indeed, fibrillating hearts have been pumped by hand for as long as 90 minutes followed by successful defibrillation.
A technique for pumping the heart without opening the chest consists of intermittent thrusts of pressure on the chest wall along with artificial respiration. This, plus defibrillation, is called cardiopulmonary resuscitation, or CPR.
Lack of blood flow to the brain for more than 5 to 8 minutes usually causes permanent mental impair-ment or even destruction of brain tissue. Even if the heart is revived, the person may die from the effects of brain damage or may live with permanent mental impairment.
Related Topics