Chapter: Clinical Dermatology: Reactive erythemas and vasculitis
Urticaria (hives, ‘nettle-rash’)
Urticaria
(hives, ‘nettle-rash’)
Urticaria
is a common reaction pattern in which pink, itchy or ‘burning’ swellings
(wheals) can occur any-where on the body. Individual wheals do not last longer
Traditionally, urticaria is divided into acute and chronic forms, based on the
duration of the disease rather than of individual wheals. Urticaria that
persists for more than 6 weeks is clas-sified as chronic. Most patients with
chronic urticaria, other than those with an obvious physical cause, have what
is often known as ‘ordinary urticaria’.
Cause
The signs and symptoms of urticaria are caused by mast cell degranulation, with release of histamine (Fig. 8.1).
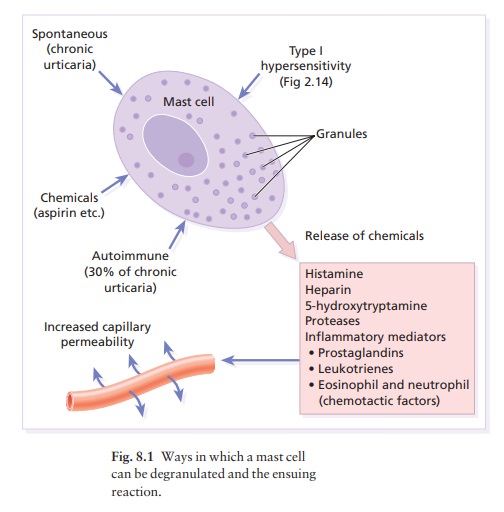
The mechanisms underlying this may be different
but the end result, increased capillary per-meability leading to transient
leakage of fluid into the surrounding tissue and development of a wheal, is the
same (Fig. 8.1). For example, up to half of those patients with chronic
urticaria have circulating anti-bodies directed against the high affinity
immuno-globulin E (IgE) receptor on mast cells whereas the reaction in others
in this group may be caused by immediate IgE-mediated hypersensitivity (see
Fig. 2.14), direct degranulation by a chemical or trauma, or even spontaneous
degranulation.
Classification
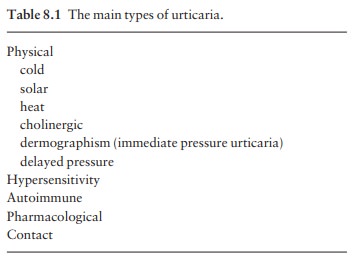
The
various types of urticaria are listed in Table 8.1. They can often be
identified by a careful history; laboratory tests are less useful. The duration
of the wheals is an important pointer. Contact and physical urticarias, with
the exception of delayed pressure urticaria, start shortly after the stimulus
and go within an hour. Individual wheals of other forms resolve within 24 h.
Physical urticarias
Cold urticaria
Patients
develop wheals in areas exposed to cold, e.g.
on
the face when cycling or freezing in a cold wind.
A useful test in the clinic is to reproduce the reac-tion by holding an ice cube, in a thin plastic bag to avoid wetting, against forearm skin. A few cases are associated with the presence of cryoglobulins, cold agglutinins or cryofibrinogens.
Solar urticaria
Wheals
occur within minutes of sun exposure. Some patients with solar urticaria have
erythropoietic protoporphyria; most have an IgE-mediated urticarial reaction to
sunlight.
Heat urticaria
In
this condition wheals arise in areas after contact with hot objects or
solutions.
Cholinergic urticaria
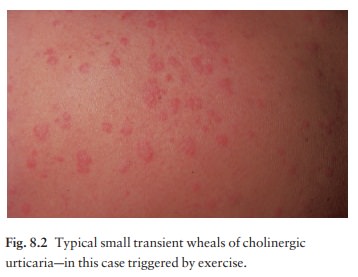
Anxiety,
heat, sexual excitement or strenuous exercise elicits this characteristic
response. The vessels over-react to acetylcholine liberated from sympathetic
nerves in the skin. Transient 2–5 mm follicular macules or papules (Fig. 8.2)
resemble a blush or viral exanthem. Some patients get blotchy patches on their
necks.
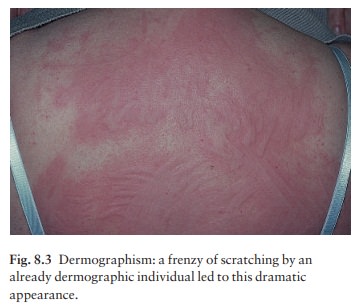
Dermographism (Fig.
8.3)
This
is the most common type of physical urticaria, the skin mast cells releasing
extra histamine after rub-bing or scratching. The linear wheals are therefore
an exaggerated triple response of Lewis. They can readily be reproduced by
rubbing the skin of the back lightly at different pressures, or by scratching
the back with a fingernail or blunt object.
Delayed pressure urticaria
Sustained pressure causes oedema of the underlying skin and subcutaneous tissue 3– 6 h later.
The swelling may
last up to 48 h and kinins or prostaglandins rather than histamine probably
mediate it. It occurs particularly on the feet after walking, on the hands
after clapping and on the buttocks after sitting. It can be disabling for
manual labourers.
Other types of urticaria
Hypersensitivity urticaria
This
common form of urticaria is caused by hyper-sensitivity, often an IgE-mediated
(type I) allergic reaction . Allergens may be encountered in ten different ways
(the 10 ‘I’s listed in Table 8.2).
Autoimmune urticaria
Some patients with chronic urticaria have an auto-immune disease with IgG antibodies to IgE or to FcIgE receptors on mast cells. Here the autoantibody acts as antigen to trigger mast cell degranulation.
Pharmacological urticaria
This
occurs when drugs cause mast cells to release histamine in a non-allergic
manner (e.g. aspirin, non-steroidal anti-inflammatory drugs (NSAIDs),
angiotensin-converting enzyme (ACE) inhibitors and morphine).
Contact urticaria
This
may be IgE-mediated or caused by a pharmaco-logical effect. Wheals occur most
often around the mouth. Foods and food additives are the most com-mon culprits
but drugs, animal saliva, caterpillars and plants may cause the reaction.
Recently, latex allergy has become a significant public health concern.
Latex allergy
Possible
reactions to the natural rubber latex of the Hevea brasiliensis tree
include irritant dermatitis, con-tact allergic dermatitis and type I allergy . Reactions associated
with the latter include hypersensitivity urticaria (both by contact and by
inhalation), hay fever, asthma, anaphylaxis and, rarely, death.
Medical
latex gloves became universally popular after precautions were introduced to
protect against HIV and hepatitis B infections. The demand for the gloves
increased and this led to alterations in their manu-facture and to a flood of
high allergen gloves on the market. Cornstarch powder in these gloves bound to
the latex proteins so that the allergen became airborne when the gloves were
put on. Individuals at increased risk of latex allergy include health care
workers, those undergoing multiple surgical procedures (e.g. spina bifida
patients) and workers in mechanical, catering and electronic trades. Around 1–
6% of the general population is believed to be sensitized to latex.
Latex reactions should be treated on their own merits. Preven-tion of latex allergy is equally important. Non-latex (e.g. vinyl) gloves should be worn by those not han-dling infectious material (e.g. caterers) and, if latex gloves are chosen for those handling infectious material, then powder-free low allergen ones should be used.
Presentation
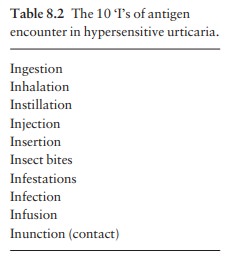
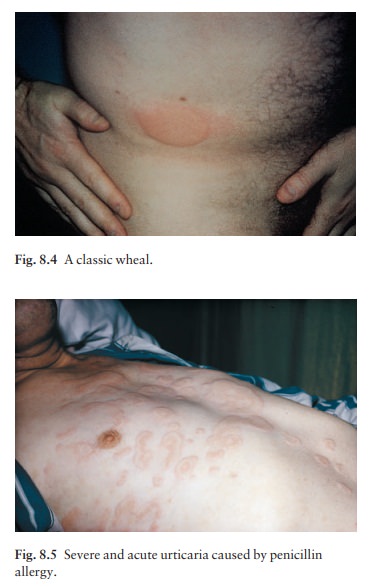
Most
types of urticaria share the sudden appear-ance of pink itchy wheals, which can
come up any-where on the skin surface (Figs 8.4 and 8.5). Each lasts for less
than a day, and most disappear within a few hours. Lesions may enlarge rapidly
and some resolve centrally to take up an annular shape. In an acute
anaphylactic reaction, wheals may cover most of the skin surface. In contrast,
in chronic urticaria only a few wheals may develop each day.
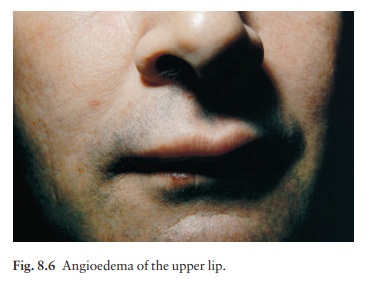
Angioedema
is a variant of urticaria that primarily affects the subcutaneous tissues, so
that the swelling is less demarcated and less red than an urticarial wheal.
Angioedema most commonly occurs at junctions between skin and mucous membranes
(e.g. peri-orbital, peri-oral and genital; Fig. 8.6). It may be associated with
swelling of the tongue and laryngeal mucosa. It sometimes accompanies chronic
urticaria and its causes may be the same.
Course
The
course of an urticarial reaction depends on its cause. If the urticaria is
allergic, it will continue until the allergen is removed, tolerated or
metabolized. Most such patients clear up within a day or two, even if the
allergen is not identified. Urticaria may recur if the allergen is met again.
At the other end of the scale, only half of patients attending hospital clinics
with chronic urticaria and angioedema will be clear 5 years later. Those with
urticarial lesions alone do better, half being clear after 6 months.
Complications
Urticaria
is normally uncomplicated, although its itch may be enough to interfere with
sleep or daily activit-ies and to lead to depression. In acute anaphylactic
reactions, oedema of the larynx may lead to asphyxi-ation, and oedema of the
tracheo-bronchial tree may lead to asthma.
Differential diagnosis
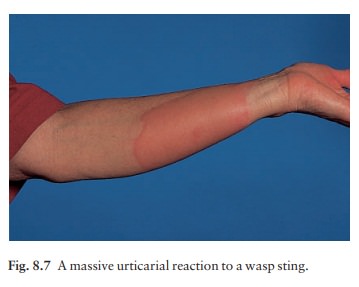
There
are two aspects to the differential diagnosis of urticaria. The first is to
tell urticaria from other eruptions that are not urticaria at all. The second
is to define the type of urticaria, according to Table 8.1. Insect bites or
stings (Fig. 8.7) and infestations com-monly elicit urticarial responses, but
these may have a central punctum and individual lesions may last longer than 24
h. Erythema multiforme can mimic an annular urticaria. A form of vasculitis
(urticarial vasculitis) may resemble urticaria, but indi-vidual lesions last
for longer than 24 h and may leave
Some bullous diseases, such as dermatitis herpetiformis, bullous
pemphigoid and pemphigoid gestationis, begin as urticarial papules or plaques,
but later bullae make the diagnosis obvious. On the face, erysipelas can be
distinguished from angioedema by its sharp margin, redder colour and
accompanying pyrexia. Hereditary angioedema must be distinguished from the
angioedema accompanying urticaria as their treatments are completely different.
Hereditary angioedema
Recurrent
attacks of abdominal pain and vomiting, or massive oedema of soft tissues,
which may involve the larynx, characterize this autosomal dominant con-dition.
Urticaria does not accompany the tissue swel-lings. Tooth extraction, cheek
biting and other forms of trauma may precipitate an attack. A deficiency of an
inhibitor to C1 esterase allows complement con-sumption to go unchecked so that
vasoactive mediators are generated. To confirm the diagnosis, serum C1 esterase
inhibitor level and C4 level should both be checked as the level of C1 esterase
inhibitor is not always depressed (there is a type where the inhibitor is
present but does not work).
Investigations
The investigations will depend upon the presentation and type of urticaria. Many of the physical urticarias can be reproduced by appropriate physical tests. It is important to remember that antihistamines should be stopped for at least 3 days before these are undertaken.
Almost
invariably, more is learned from the history than from the laboratory. The
history should include details of the events surrounding the onset of the
erup-tion. A review of systems may uncover evidence of an underlying disease.
Careful attention should be paid to drugs, remembering that self-prescribed
ones can also cause urticaria. Over-the-counter medications (such as aspirin
and herbal remedies) and medications given by other routes (Table 8.2) can
produce wheals.
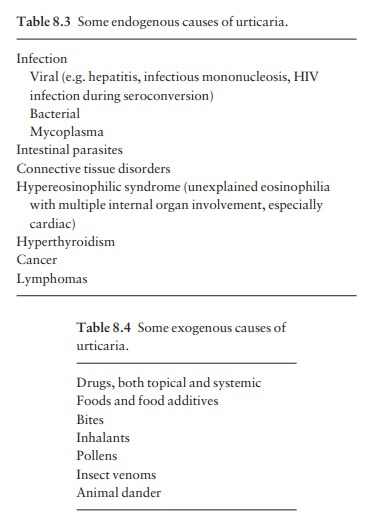
If
a patient has acute urticaria and its cause is not obvious, investigations are
often deferred until it has persisted for a few weeks; then a physical
examination (if not already carried out) and screening tests such as a complete
blood count, erythrocyte sedimentation rate (ESR), routine biochemical screen,
chest X-ray and urine analysis are worthwhile. If the urticaria continues for
2–3 months, the patient should prob-ably be referred to a dermatologist for
further evalu-ation. In general, the focus of such investigations will be on
internal disorders associated with urticaria (Table 8.3) and on external
allergens (Table 8.4). Even after extensive evaluation and environmental
change, the cause cannot always be found.
In
some patients with acute or contact urticaria, allergy testing in the form of
radioallergosorbant tests (RAST) or prick tests , using only allergens
suggested by the history, can sometimes be of help. Many patients with chronic
urticaria are sure that their problems could be solved by intensive allergy
tests, and ask repeatedly for them, but this is seldom worthwhile.
Treatment
The
ideal is to find a cause and then to eliminate it. In addition, aspirinain any
formashould be banned. The treatment for each type of urticaria is outlined in
Table 8.5. In general, antihistamines are the mainstays of symptomatic
treatment. Cetirizine 10 mg/day and loratadine 10 mg/day, both with half-lives
of around 12 h, are useful. If necessary, these can be supplemented
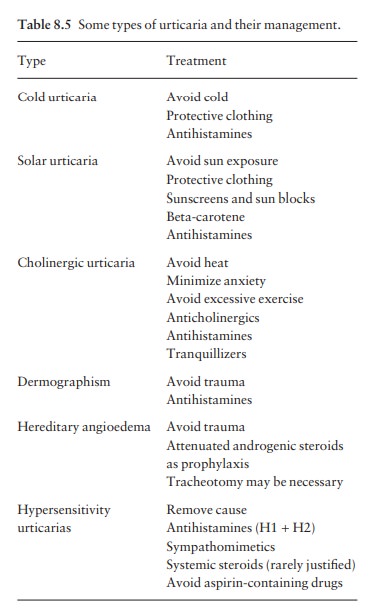
Alternatively they can
be combined with a longer acting antihistamine (such as chlorpheniramine
maleate 12 mg sustained-release tablets every 12 h) so that peaks and troughs
are blunted, and histamine activity is blocked throughout the night. If the
eruption is not controlled, the dose of hydroxyzine can often be increased and
still tolerated. H2-blocking antihistamines (e.g. cimetidine) may add a slight
benefit if used in conjunction with an H1 histamine antagonist.
Chlorpheniramine or diphen-hydramine are often used during pregnancy because of
their long record of safety, but cetirizine, loratidine and mizolastine should
be avoided. Sympathomimetic agents can help urticaria, although the effects of
adrena-line (epinephrine) are short lived. Pseudoephedrine (30 or 60 mg every 4
h) or terbutaline (2.5 mg every 8 h) can sometimes be useful adjuncts.
A
tapering course of systemic corticosteroids may be used, but only when the
cause is known and there are no contraindications, and certainly not as a
panacea to control chronic urticaria or urticaria of unknown cause. For the
treatment of anaphylaxis.
Related Topics