Chapter: Clinical Dermatology: Reactive erythemas and vasculitis
Leucocytoclastic
Leucocytoclastic (small vessel) vasculitis (Syn: allergic or hypersensitivity vasculitis, anaphylactoid purpura)
Cause
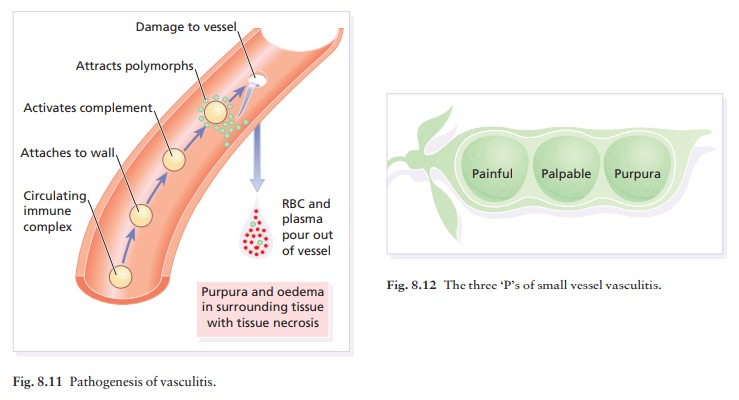
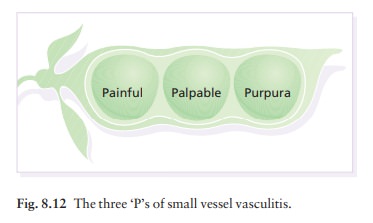
Immune
complexes may lodge in the walls of blood vessels, activate complement and
attract polymor-phonuclear leucocytes (Fig. 8.11). Enzymes released from these
can degrade the vessel wall. Antigens in these immune complexes include drugs,
auto-antigens, and infectious agents such as bacteria.
Presentation
The most common presentation of vasculitis is painful palpable purpura (Fig. 8.12). Crops of lesions arise in dependent areas (the forearms and legs in ambulatory patients, or on the buttocks and flanks in bedridden ones; Fig. 8.13). Some have a small, livid or black centre, caused by necrosis of the tissue overlying the affected blood vessel.

Henoch–Schönlein
purpura is a small vessel vas-culitis associated with palpable purpura,
arthritis and abdominal pain, often preceded by an upper respirat-ory tract
infection. Children are most commonly, but not exclusively, affected.
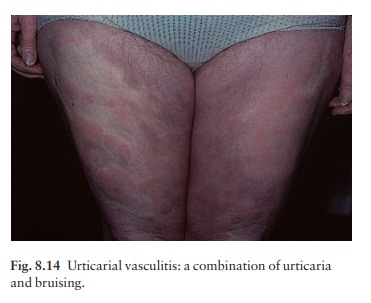
Urticarial vasculitis is a small vessel vasculitis char-acterized by urticaria-like lesions which last for longer than 24 h, leaving bruising and then pigmentation (haemosiderin) at the site of previous lesions (Fig. 8.14). There may be foci of purpura in the wheals and other skin signs include angioedema. General features include malaise and arthralgia.
Course
The
course of the vasculitis varies with its cause, its extent, the size of blood
vessel affected, and the involvement of other organs.
Complications
Vasculitis
may simply be cutaneous; alternatively, it may be systemic and then other
organs will be damaged, including the kidney, central nervous sys-tem,
gastrointestinal tract and lungs.
Differential diagnosis
Small
vessel vasculitis has to be separated from other causes of purpura such as abnormalities of the clotting system
and sepsis (with or without vasculitis). Vasculitic purpuras are raised
(palpable). Occasionally, the vasculitis may look like urticaria if its purpuric
element is not marked. Blanching such an urticarial papule with a glass slide
may reveal subtle purpura.
Investigations
Investigations
should be directed toward identifying the cause and detecting internal
involvement. Ques-tioning may indicate infections; myalgias, abdominal pain,
claudication, mental confusion and mononeuritis may indicate systemic
involvement. A physical examination, chest X-ray, ESR and biochemical tests
mon-itoring the function of various organs are indicated. However, the most
important test is urine analysis, checking for proteinuria and haematuria,
because vasculitis can affect the kidney subtly and so lead to renal
insufficiency.
Skin
biopsy will confirm the diagnosis of small vessel vasculitis. The finding of
circulating immune complexes, or a lowered level of total complement (CH50) or
C4, will implicate immune complexes as its cause. Tests for hepatitis virus,
cryoglobulins, rheumatoid factor and antinuclear antibodies may also be needed.
Direct
immunofluorescence can be used to identify immune complexes in blood vessel
walls, but is seldom performed because of false-positive and false-negative
results, as inflammation may destroy the complexes in a true vasculitis and
induce non-specific deposition in other diseases. Henoch–Schönlein vasculitis
is con-firmed if IgA deposits are found in the blood vessels of a patient with
the clinical triad of palpable purpura, arthritis and abdominal pain.
Treatment
The
treatment of choice is to identify the cause and eliminate it. In addition,
antihistamines and bed rest sometimes help. Colchicine 0.6 mg twice daily or
dapsone 100 mg daily may be worth a trial, but require monitoring for
side-effects. Pati-ents whose vasculitis is damaging the kidneys or other
internal organs may require systemic corticosteroids or immunosuppressive
agents such as cyclophosphamide.
Related Topics