Chapter: Medicine and surgery: Gastrointestinal system
Ulcerative colitis - Disorders of the large bowel and inflammatory bowel disease
Ulcerative colitis
Definition
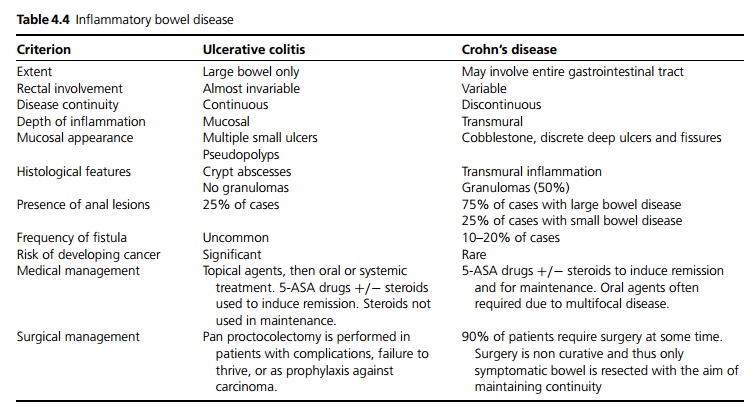
Chronic inflammatory bowel disease affecting only the large bowel, characterised by the formation of crypt abscesses (see Table 4.4).
Incidence
5 per 100,000 per year.
Age
Peak in young adult life.
Sex
F > M
Aetiology
Multifactorial aetiology including
1. Familial: Familial tendency, some concordance between monozygotic twins.
2. Genetic: HLA B27 is more common in patients.
3. Smoking: Patients presenting with ulcerative colitis are more likely to be non-smokers or recent exsmokers.
4. Immunological: pANCA may be found in ulcerative colitis.
Pathophysiology
Ulcerative colitis is characterised by continuous inflammation starting in the rectum (proctitis) and extending variably to the descending colon or there may be a total colitis (pancolitis). In a few patients inflammation of the distal terminal ileum occurs termed backwash ileitis.
Clinical features
The condition is characterised by acute exacerbations interspersed by clinical remission. In acute episodes, patients present with diarrhoea containing blood and mucous which may be copious and associated with urgency. There may be extragastrointestinal features including erythema nodosum and pyoderma gangrenosum in the skin, iritis, arthropathy of large joints, sacroiliitis and ankylosing spondylitis (HLA B27) and chronic liver disease.
Macroscopy/microscopy
1. During acute exacerbation there is superficial mucosal haemorrhagic ulceration, interspersed with more normal mucosa appearing as an inflammatory polyp (pseudopolyps). On microscopy there is oedema and lymphocytic infiltration of the lamina propria. Neutrophils migrate through the wall of mucosal glands to form crypt abscesses.
2. During remission there is little ulceration, the mucosa appears hyperaemic and thin. Microscopy reveals chronic inflammatory cell infiltration.
3. Confluent inflammation and ulceration extending into the muscle layer is seen in fulminant disease.
Complications
Severe fulminant disease may manifest as toxic colonic dilation, septicaemia, obstruction and perforation. Chronic bowel inflammation is associated with increased risk of cellular dysplasia and a significant risk of carcinoma.
Investigations
Anaemia due to blood loss, iron deficiency or chronic disease, acute inflammation may also cause a rise in platelet count. Inflammatory markers such as ESR are often raised in acute exacerbations.
Barium enema may cause perforation in acute disease and is therefore contraindicated. In mild disease a diffusely reticulated pattern is seen with punctate collections of barium in small ulcers. In chronic disease a featureless colon with complete loss of folds is seen. Repeated plain abdominal X-ray is of value in acute flares to diagnose acute colonic dilation.
Colonosocopy with biopsy is diagnostic but may induce megacolon or perforation in severe, extensive disease. Flexible sigmoidoscopy is safer and usually adequate.
Stool culture and microscopy is used to exclude additional infection.
Management
1. Mild attacks of proctitis or proctosigmoiditis can be treated topically with 5-aminosalicylic acid (5-ASA) suppositories or enemas or steroid enemas. If these are not tolerated, or if there is involvement of more of the colon, oral 5-ASA or steroids may also be used.
2. Severe attacks or fulminant colitis should be treated with high dose steroids (oral or intravenous). Fluid and antibiotic management is often required. Ciclosporin may induce remissions in refractory attacks.
3. Maintenance therapy is with low dose 5-aminosalicylic acid. Steroids can maintain remission but due to long term side effects steroid sparing agents such as azathioprine are often used. Azathioprine requires careful monitoring as it may cause abnormal liver function tests or bone marrow suppression. Azathioprine should be avoided in patients who are TPMT (thiopurine-S-methyltransferase) deficient as they are at particular risk of bone marrow suppression.
4. Alternative treatments: Intravenous heparin and nicotine patches have been shown in some studies to help induction of remission in refractory UC, but are not recommended as maintenance therapy.
· Surgical treatment: Panproctocolectomy with permanent ileostomy involves removal of all the colonic mucosa and is curative.
· Colectomy and ileorectal anastomosis does not require ileostomy but proctitis may persist causing diarrhoea and cancer surveillance is still necessary.
· Pan colectomy with retention of the anal sphincters allows anastomosis via an ileal pouch. This removes all diseased mucosa.
· Emergency surgery for perforation, toxic dilation, massive bleeding and refractory severe exacerbations may be necessary but carries a significant mortality.
Prognosis
Relapses and remissions with overall prognosis related to the extent of the disease. 3–5% of patients with UC develop colonic carcinoma, the risk is much greater in those with active disease for more than 10 years.
Related Topics