Chapter: Medical Surgical Nursing: Critical Thinking,Ethical Decision Making, and the Nursing Process
Types of Ethical Problems in Nursing
TYPES
OF ETHICAL PROBLEMS IN NURSING
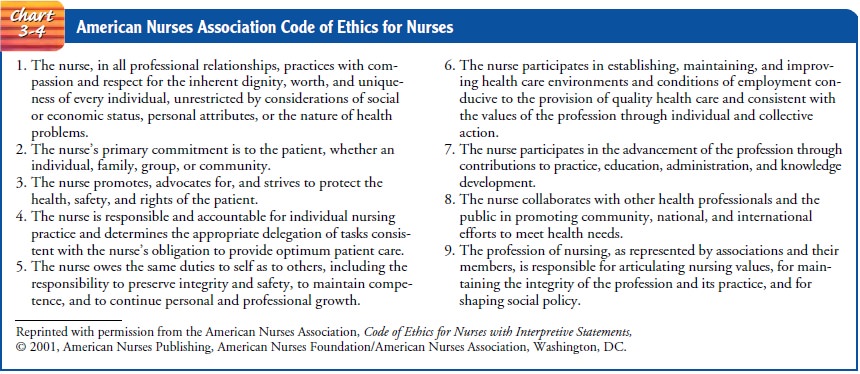
As a profession, nursing
is accountable to society. This account-ability is spelled out in the American
Hospital Association’s Patient Care Partnership (Chart 3-3), which reflects
social beliefs about health and health care. In addition to accepting this
document as one measure of accountability, nursing has further defined its
standards of accountability through a formal code of ethics that explicitly
states the profession’s values and goals. The code (Chart 3-4), established by
the American Nurses Association (ANA), consists of ethical standards, each with
its own interpre-tive statements (ANA, 2001). The interpretive statements
provide guidance to address and resolve ethical dilemmas by incorporating
universal moral principles (ANA’s Code of Ethics Project Task Force, 2000). The
code is an ideal framework for nurses to use in ethical decision making.

Ethical issues have
always affected the role of the professional nurse. The accepted definition of
professional nursing has inspired a new advocacy role for nurses. The ANA, in Nursing’s Social Pol-icy Statement (1995),
defines nursing as “the diagnosis and treat-ment of human responses to health
and illness.” This definition supports the claim that nurses must be actively
involved in the decision-making process regarding ethical concerns surrounding
health care and human responses. Efforts to enact this standard may cause
conflict in health care settings in which the traditional roles of the nurse
are delineated within a bureaucratic structure. If, however, nurses learn to present
ethical conflicts within a logi-cal, systematic framework, struggles over
jurisdictional boundaries may decrease. Health care settings in which nurses
are valued members of the team promote interdisciplinary communication and may
enhance patient care. To practice effectively in these set-tings, nurses must
be aware of ethical issues and assist patients in voicing their moral concerns.
The basic ethical
framework of the nursing profession is the phenomenon of human caring. Nursing
theories that incorporate the biopsychosocial–spiritual dimensions emphasize a
holistic viewpoint, with humanism or caring as the core. As the nursing
profession strives to delineate its own theory of ethics, caring is often cited
as the moral foundation. For nurses to embrace this professional ethos, it is
necessary to be aware not only of major ethical dilemmas but also of those
daily interactions with health care consumers that frequently give rise to
ethical challenges that are not as easily identified. Although technological
advances and diminished resources have been instrumental in raising numer-ous
ethical questions and controversies, including life-and-death issues, nurses
should not ignore the many routine situations that involve ethical
considerations. Some of the most common issues faced by nurses today include
confidentiality, use of restraints, trust, refusing care, genetics, and
end-of-life concerns.
Confidentiality
We all need to be aware
of the confidential nature of information obtained in daily practice. If information
is not pertinent to a case, the nurse should question whether it is prudent to
record it in the patient’s chart. In the practice setting, discussion of the
pa-tient with other members of the health care team is often neces-sary. These
discussions should, however, occur in a private area where it is unlikely that
the conversation will be overheard.
Another threat to
keeping information confidential is the widespread use of computers and the
easy access people have to them. This may increase the potential for misuse of
information, which may have negative social consequences (Zolot, 1999). For
example, laboratory results regarding testing for human immuno-deficiency virus
(HIV) infection or genetic screening may lead to loss of employment or insurance
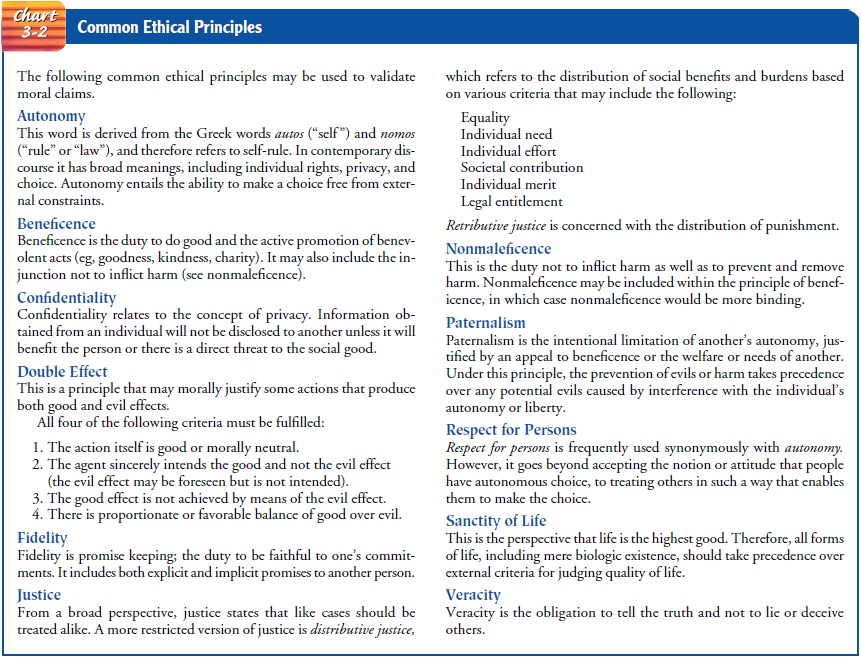
if the information is disclosed. Because of these possibilities of maleficence
(see Chart 3-2) to the patient, sensitivity to the principle of confidentiality
is essential.
Restraints
The use of restraints
(including physical and pharmacologic mea-sures) is another issue with ethical
overtones. It is important to weigh carefully the risks of limiting a person’s
autonomy and in-creasing the risk of injury by using restraints against the
risks of not using restraints. Before restraints are used, other strategies,
such as asking family members to sit with the patient, should be tried (Rogers
& Bocchino, 1999). The Joint Commission on Accredi-tation of Healthcare
Organizations (JCAHO) and the Health Care Financing Administration (HCFA) have
designated standards for use in care of patients with restraints; these
standards are available on the website listed later.
Trust Issues
Telling the truth (veracity) is one of the basic principles of our culture. Two ethical dilemmas in clinical practice that can di-rectly conflict with this principle are the use of placebos (non-active substances used to treat symptoms) and not revealing a di-agnosis to the patient. Both involve the issue of trust, which is an essential element in the nurse–patient relationship. Placebos may be used in experimental research, where the patient is involved in the decision-making process and is aware that placebos are being used in the treatment regimen. However, the use of a placebo as a substitute for an active drug to show that the patient does not have real symptoms is deceptive. This practice may severely un-dermine the nurse–patient relationship.
Informing patients of their diagnoses when the family and physician have chosen to withhold information is a common eth-ical situation in nursing practice. The nursing staff often use evasive comments with the patient as a means to maintain profes-sional relationships with other health practitioners.
This area is in-deed complex because it challenges the nurse’s integrity. Trust and connection with the patient play an important part in optimizing care (Day & Stannard, 1999). Strategies the nurse could consider in this situation include the following:
• Not lying to the patient
• Providing all information related to nursing procedures and diagnoses
• Communicating to the family and physician the patient’s requests for information
Families often are unaware of the patient’s repeated questions to the nurse. With a better understanding of the situation, fami-lies may change their perspective. Finally, although providing the information may be the morally appropriate behavior, the man-ner in which the patient is told is important. Nurses must be compassionate and caring while informing patients; disclosure of information merely for the sake of patient autonomy does not convey respect for others.
Refusing to Provide Care
Any nurse who feels compelled to refuse to provide care for a par-ticular type of patient faces an ethical dilemma. The reasons given for refusal range from a conflict of personal values to fear of per-sonal risk of injury. Such instances have increased since the ad-vent of acquired immunodeficiency syndrome (AIDS) as a major health problem. In one survey, the number of nurses who stated they might refuse to care for a patient with AIDS declined over a 10-year period, from 75% to 20%. The number who might refuse to care for a patient with AIDS who was violent or uncooperative, however, rose from 72% to 82% (Ventura, 1999).
The ethical obligation to care for all patients is clearly identified in the first statement of the Code of Ethics for Nurses. To avoid facing these moral situations, a nurse can follow certain strategies. For example, when applying for a job, one should ask questions re-garding the patient population. If one is uncomfortable with a par-ticular situation, then not accepting the position would be an option. Denial of care, or providing substandard nursing care to some members of our society, is not acceptable nursing practice.
End-of-Life Issues
Dilemmas that center on death
and dying are prevalent in medical-surgical nursing practice and frequently
initiate moral discussion. The dilemmas are compounded by the fact that the
idea of curing is paramount in health care. With advanced technology, it may be
difficult to accept the fact that nothing more can be done, or that technology
may prolong life but at the expense of comfort and quality of life. Focusing on
the caring as well as the curing role may assist nurses in dealing with these
difficult moral situations.
PAIN CONTROL
The use of opioids to alleviate a patient’s pain may present a dilemma
for nurses. Patients with excruciating pain may require large doses of
analgesics. Fear of respiratory depression or un-warranted fear of addiction
should not prevent nurses from at-tempting to alleviate pain for the dying
patient or for a patient experiencing an acute pain episode. In the case of the
terminally ill patient, for example, the actions may be justified by the
princi-ple of double effect (see Chart 3-2). The intent or goal of nursing
interventions is to alleviate pain and suffering while promoting comfort. The
risk of respiratory depression is not the intent of the actions and should not
be used as an excuse for withholding anal-gesia. However, the patient’s
respiratory status should be carefully monitored and any signs of respiratory
depression reported to the physician. The administration of analgesia should be
governed by the patient’s needs.
DO-NOT-RESUSCITATE ORDERS
The “do not resuscitate” (DNR) order is a controversial issue. When a
patient is competent to make decisions, his or her choice for a DNR order
should be honored, according to the principles of autonomy or respect for the
individual (Trammelleo, 2000). However, a DNR order is at times interpreted to
mean that the patient requires less nursing care, when actually these patients
may have significant medical and nursing needs, all of which de-mand attention.
Ethically, all patients deserve and should receive appropriate nursing
interventions, regardless of their resuscita-tion status.
LIFE SUPPORT
In contrast to the
previous situations are those in which a DNR decision has not been made by or
for a dying patient. The nurse may be put in the uncomfortable position of
initiating life-support measures when, because of the patient’s physical
condition, they appear futile. This frequently occurs when the patient is not
competent to make the decision and the family (or surrogate de-cision maker)
refuses to consider a DNR order as an option. The nurse may be told to perform
a “slow code” (ie, not to rush to re-suscitate the patient) or may be given a
verbal order not to resus-citate the patient; both are unacceptable medical
orders. The best recourse for nurses in these situations is to be aware of
hospital policy related to the Patient Self-Determination Act (discussed later)
and execution of advance directives. The nurse should communicate with the
physician. Discussing the matter with the physician may lead to further
communication with the family and to a reconsideration of their decision,
especially if they are afraid to let a loved one die with no further efforts to
resuscitate (Trammelleo, 2000). Finally, when working with colleagues who are
confronting such difficult situations, it helps to talk and lis-ten to their
concerns as a way of providing support.
FOOD AND FLUID
In addition to
requesting that no heroic measures be taken to pro-long life, a dying patient
may request that no more food or fluid be administered. Many individuals think
that food and hydration are basic human needs, not “invasive measures,” and
therefore should always be maintained. However, some consider food and
hydration as means of prolonging suffering. In evaluating this issue, nurses
must take into consideration the potential harm as well as the benefit to the
patient of either administering or with-drawing sustenance. Research has not
supported the belief that withholding fluids results in a painful death due to
thirst (Smith, 1997; Zerwekh, 1997).
Evaluation of harm
requires a careful review of the reasons the person has requested the
withdrawal of food and hydration. Although the principle of autonomy has
considerable merit and is supported by the Code of Ethics for Nurses, there may
be sit-uations when the request for withdrawal of food and hydration cannot be
upheld. For patients with decreased decision-making capacity, the issues are
more complex. Some of these cases have reached courts of law, and different
states have different case law precedents forbidding withdrawal of sustenance.
Although an ad-vance directive may provide some answers, at present there are
no firm guidelines to assist nurses in this area.
Related Topics