Chapter: Medical Surgical Nursing: Critical Thinking,Ethical Decision Making, and the Nursing Process
Domain of Nursing Ethics
Domain of Nursing Ethics
The ethical dilemmas a
nurse may encounter in the medical-surgical arena are numerous and diverse. An
awareness of under-lying philosophical concepts will help the nurse to reason
through these dilemmas. Basic concepts related to moral philosophy, such as
ethics terminology, theories, and approaches. Understanding the role of the
professional nurse in ethical decision making will assist nurses in
articulating their ethical posi-tions and in developing the skills needed to
make ethical decisions.
ETHICS VERSUS MORALITY
The terms ethics and morality are used to describe beliefs about right and wrong and to
suggest appropriate guidelines for action. In essence, ethics is the formal,
systematic study of moral beliefs, whereas morality is the adherence to
informal personal values. Because the distinction between the two is slight,
they are often used interchangeably.
ETHICS THEORIES
One classic theory in
ethics is teleologic theory or consequential-ism, which focuses on the ends or
consequences of actions. The most well-known form of this theory,
utilitarianism, is based on the concept of “the greatest good for the greatest
number.” The choice of action is clear under this theory, because the action
that maximizes good over bad is the correct one. The theory poses dif-ficulty
when one must judge intrinsic values and determine whose good is the greatest.
Additionally, the question must be asked whether good consequences can justify
any amoral actions that might be used to achieve them.
Another theory in ethics
is the deontologic or formalist theory, which argues that moral standards or
principles exist independently of the ends or consequences. In a given
situation, one or more moral principles may apply. The nurse has a duty to act
based on the one relevant principle, or the most relevant of several moral
principles. Problems arise with this theory when personal and cultural biases
influence the choice of the most primary moral principle.
APPROACHES TO ETHICS
Two approaches to ethics
are metaethics and applied ethics. An example of metaethics (understanding the
concepts and linguis-tic terminology used in ethics) in the health care
environment would be analysis of the concept of informed consent. Nurses are
aware that patients must give consent before surgery, but some-times a question
arises as to whether the patient is truly informed. Delving more deeply into
the concept of informed consent would be a metaethical inquiry.
Applied ethics is the
term used when questions are asked of a specific discipline to identify ethical
problems within that disci-pline’s practice. Various disciplines use the
frameworks of general ethical theories and moral principles and apply them to
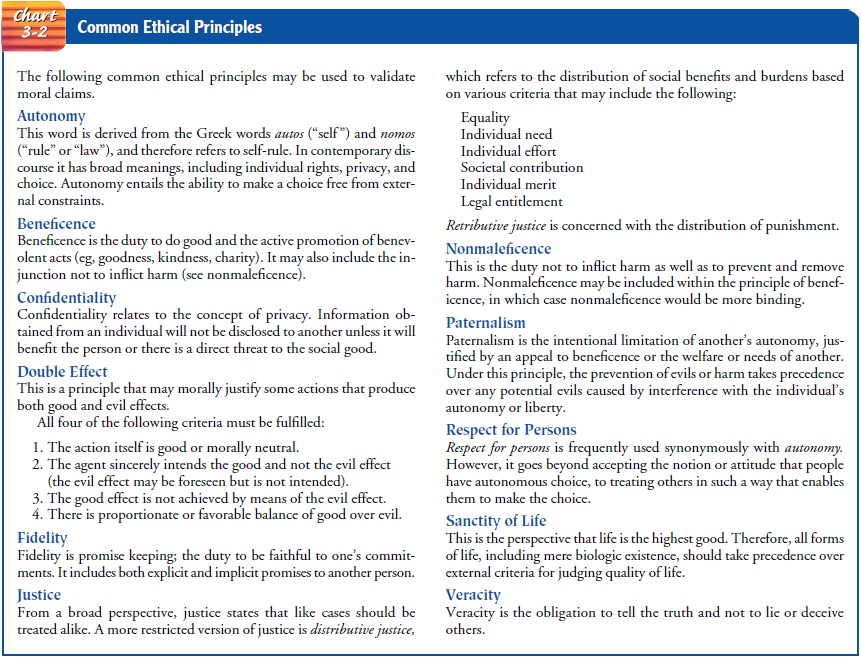
specific problems within their domain. Common ethical principles that apply in
nursing include autonomy, beneficence, confidentiality, double effect,
fidelity, justice, nonmaleficence, paternalism, re-spect for people, sanctity
of life, and veracity. Brief definitions of these important principles can be
found in Chart 3-2.
Nursing ethics may be
considered a form of applied ethics be-cause it addresses moral situations that
are specific to the nursing profession and patient care. Some ethical problems
that affect nursing may also apply to the broader area of bioethics and health
care ethics. However, the nursing profession is a “caring” rather than a
predominantly “curing” profession; therefore, it is imperative that one not
equate nursing ethics solely with medical ethics, because the medical
profession has a “cure” focus. Nursing has its own professional code of ethics.
MORAL SITUATIONS
Many situations exist in
which ethical analysis is needed. Some are moral
dilemmas, situations in which a clear conflict exists betweentwo or more
moral principles or competing moral claims, and the nurse must choose the
lesser of two evils. Other situations repre-sent moral problems, in which there may be competing moral claims or
principles but one claim or principle is clearly dominant. Some situations
result in moral uncertainty, when one
cannot accurately define what the moral situation is, or what moral principles
apply, but has a strong feeling that something is not right. Still other
sit-uations may result in moral distress,
in which the nurse is aware of the correct course of action but institutional
constraints stand in the way of pursuing the correct action (Jameton, 1984).
For example, a patient
tells a nurse that if he is dying he wants everything possible done. The surgeon
and family have made the decision not to tell the patient he is terminally ill
and not to re-suscitate him if he stops breathing. From an ethical perspective,
patients should be told the truth about their diagnoses and should have the
opportunity to make decisions about treatments. Ideally, this information
should come from the physician, with the nurse present to assist the patient in
understanding the terminology and to provide further support, if necessary. A
moral problem exists because of the competing moral claims of the family and
physi-cian, who wish to spare the patient distress, and the nurse, who wishes
to be truthful with the patient as the patient has requested. If the patient’s
competency were questionable, a moral dilemma would exist because no dominant
principle would be evident. The nurse could experience moral distress if the
hospital threatens dis-ciplinary action or job termination if the information
is disclosed without the agreement of the physician or the family, or both.
It is essential that
nurses freely engage in dialogue concerning moral situations, even though such
dialogue is difficult for every-one involved. Improved interdisciplinary
communication is sup-ported when all members of the health care team can voice
their concerns and come to an understanding of the moral situation. The use of
an ethics consultant or consultation team could be helpful to assist the health
care team, patient, and family to iden-tify the moral dilemma and possible
approaches to the dilemma. The nurse should be familiar with agency policy
supporting pa-tient self-determination and resolution of ethical issues. The
nurse should be an advocate for patient rights in each situation (Trammelleo,
2000).
TYPES OF ETHICAL PROBLEMS IN NURSING
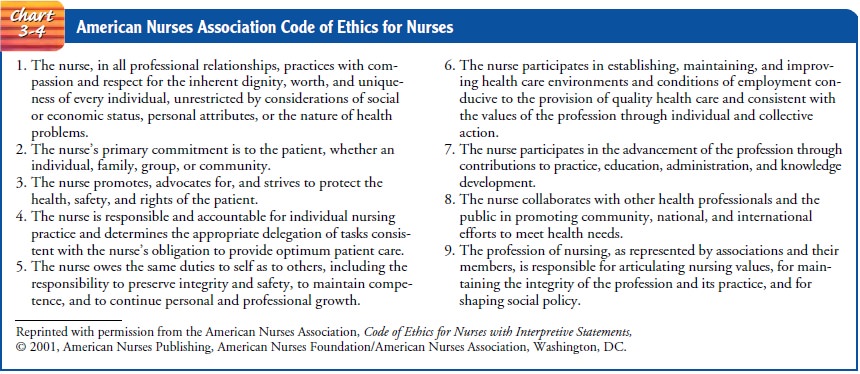
As a profession, nursing
is accountable to society. This account-ability is spelled out in the American
Hospital Association’s Patient Care Partnership (Chart 3-3), which reflects
social beliefs about health and health care. In addition to accepting this
document as one measure of accountability, nursing has further defined its
standards of accountability through a formal code of ethics that explicitly
states the profession’s values and goals. The code (Chart 3-4), established by
the American Nurses Association (ANA), consists of ethical standards, each with
its own interpre-tive statements (ANA, 2001). The interpretive statements
provide guidance to address and resolve ethical dilemmas by incorporating
universal moral principles (ANA’s Code of Ethics Project Task Force, 2000). The
code is an ideal framework for nurses to use in ethical decision making.

Ethical issues have
always affected the role of the professional nurse. The accepted definition of
professional nursing has inspired a new advocacy role for nurses. The ANA, in Nursing’s Social Pol-icy Statement (1995),
defines nursing as “the diagnosis and treat-ment of human responses to health
and illness.” This definition supports the claim that nurses must be actively
involved in the decision-making process regarding ethical concerns surrounding
health care and human responses. Efforts to enact this standard may cause
conflict in health care settings in which the traditional roles of the nurse
are delineated within a bureaucratic structure. If, however, nurses learn to present
ethical conflicts within a logi-cal, systematic framework, struggles over
jurisdictional boundaries may decrease. Health care settings in which nurses
are valued members of the team promote interdisciplinary communication and may
enhance patient care. To practice effectively in these set-tings, nurses must
be aware of ethical issues and assist patients in voicing their moral concerns.
The basic ethical
framework of the nursing profession is the phenomenon of human caring. Nursing
theories that incorporate the biopsychosocial–spiritual dimensions emphasize a
holistic viewpoint, with humanism or caring as the core. As the nursing
profession strives to delineate its own theory of ethics, caring is often cited
as the moral foundation. For nurses to embrace this professional ethos, it is
necessary to be aware not only of major ethical dilemmas but also of those
daily interactions with health care consumers that frequently give rise to
ethical challenges that are not as easily identified. Although technological
advances and diminished resources have been instrumental in raising numer-ous
ethical questions and controversies, including life-and-death issues, nurses
should not ignore the many routine situations that involve ethical
considerations. Some of the most common issues faced by nurses today include
confidentiality, use of restraints, trust, refusing care, genetics, and
end-of-life concerns.
Related Topics