Chapter: Medical Physiology: Insulin, Glucagon, and Diabetes Mellitus
Type II Diabetes-Resistance to the Metabolic Effects of Insulin
Type II Diabetes-Resistance to the Metabolic Effects of Insulin
Type II diabetes is far more common than type I, accounting for about 90 per cent of all cases of diabetes mellitus. In most cases, the onset of type II diabetes occurs after age 30, often between the ages of 50 and 60 years, and the disease develops gradually.Therefore, this syndrome is often referred to as adult-onset diabetes. In recent years, however, there has been a steady increase in the number of younger individuals, some less than 20 years old, with type II diabetes. This trend appears to be related mainly to the increasing prevalence of obesity, the most important risk factor for type II diabetes in chil-dren as well as in adults.
Obesity, Insulin Resistance, and “Metabolic Syndrome” Usually Precede Development of Type II Diabetes. Type II diabetes, incontrast to type I, is associated with increased plasma insulin concentration (hyperinsulinemia). This occurs as a compensatory response by the pancreatic beta cells for diminished sensitivity of target tissues to the meta-bolic effects of insulin, a condition referred to asinsulinresistance. The decrease in insulin sensitivity impairscarbohydrate utilization and storage, raising blood glucose and stimulating a compensatory increase in insulin secretion.
Development of insulin resistance and impaired glucose metabolism is usually a gradual process, begin-ning with excess weight gain and obesity. The mecha-nisms that link obesity with insulin resistance, however, are still uncertain. Some studies suggest that there are fewer insulin receptors, especially in the skeletal muscle, liver, and adipose tissue, in obese than in lean subjects. However, most of the insulin resistance appears to be caused by abnormalities of the signaling pathways that link receptor activation with multiple cellular effects. Impaired insulin signaling appears to be closely related to toxic effects of lipid accumulation in tissues such as skeletal muscle and liver secondary to excess weight gain.
Insulin resistance is part of a cascade of disorders that is often called the “metabolic syndrome.” Some of the features of the metabolic syndrome include: (1) obesity, especially accumulation of abdominal fat; (2) insulin resistance; (3) fasting hyperglycemia; (4) lipid abnor-malities such as increased blood triglycerides and decreased blood high-density lipoprotein-cholesterol; and (5) hypertension. All of the features of the meta-bolic syndrome are closely related to excess weight gain, especially when it is associated with accumulation of adipose tissue in the abdominal cavity around the vis-ceral organs.
The role of insulin resistance in contributing to some of the components of the metabolic syndrome is unclear, although it is clear that insulin resistance is the primary cause of increased blood glucose concentra-tion. The major adverse consequence of the metabolic syndrome is cardiovascular disease, including athero-sclerosis and injury to various organs throughout the body. Several of the metabolic abnormalities associated with the syndrome are risk factors for cardiovascular disease, and insulin resistance predisposes to the devel-opment of type II diabetes mellitus, also a major cause of cardiovascular disease.
Other Factors That Can Cause Insulin Resistance and Type II Dia- betes. Although most patients with type II diabetes areoverweight or have substantial accumulation of visceral fat, severe insulin resistance and type II diabetes can also occur as a result of other acquired or genetic con-ditions that impair insulin signaling in peripheral tissues (Table 78–2).
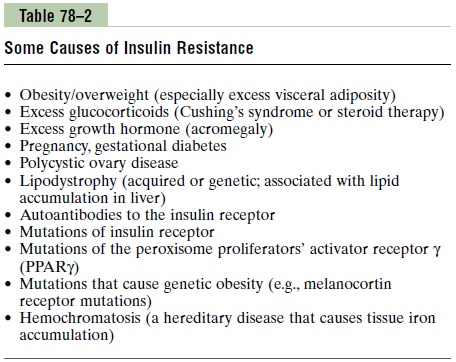
Polycystic ovary syndrome (PCOS), for example, isassociated with marked increases in ovarian androgen production and insulin resistance and is one of the most common endocrine disorders in women, affecting ap-proximately 6 per cent of all women during their re-productive life. Although the pathogenesis of PCOS remains uncertain, insulin resistance and hyperinsuline-mia are found in approximately 80 per cent of affected women. The long-term consequences include increased risk for diabetes mellitus, increased blood lipids, and cardiovascular disease.
Excess formation of glucocorticoids (Cushing’s syn-drome) or growth hormone (acromegaly) also decreasesthe sensitivity of various tissues to the metabolic effects of insulin and can lead to development of diabetes mel-litus. Genetic causes of obesity and insulin resistance, if severe enough, also can lead to type II diabetes as well as many other features of the metabolic syndrome, including cardiovascular disease.
Development of Type II Diabetes During Prolonged Insulin Resis- tance. With prolonged and severe insulin resistance,even the increased levels of insulin are not sufficient to maintain normal glucose regulation. As a result, mod-erate hyperglycemia occurs after ingestion of carbohy-drates in the early stages of the disease.
In the later stages of type II diabetes, the pancreatic beta cells become “exhausted” and are unable to produce enough insulin to prevent more severe hyperglycemia, especially after the person ingests a carbohydrate-rich meal.
Some obese people, although having marked insulin resistance and greater than normal increases in blood glucose after a meal, never develop clinically significant diabetes mellitus; apparently, the pancreas in these people produces enough insulin to prevent severe abnormalities of glucose metabolism. In others, however, the pancreas gradually becomes exhausted from secreting large amounts of insulin, and full-blown diabetes mellitus occurs. Some studies suggest that genetic factors play an important role in determining whether an individual’s pancreas can sustain the high output of insulin over many years that is necessary to avoid the severe abnormalities of glucose metabolism in type II diabetes.
In many instances, type II diabetes can be effectively treated, at least in the early stages, with exercise, caloric restriction, and weight reduction, and no exogenous insulin administration is required. Drugs that increase insulin sensitivity, such as thiazolidinediones andmet-formin, or drugs that cause additional release of insulinby the pancreas, such as sulfonylureas, may also be used. However, in the later stages of type II diabetes, insulin administration is usually required to control plasma glucose.
Related Topics