Chapter: Medical Physiology: Insulin, Glucagon, and Diabetes Mellitus
Physiology of Diagnosis of Diabetes Mellitus
Physiology of Diagnosis of Diabetes Mellitus
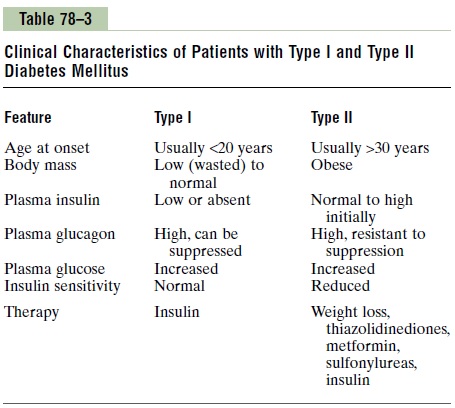
Table 78–3 compares some of clinical features of type I and type II diabetes mellitus. The usual methods for diagnosing diabetes are based on various chemical tests of the urine and the blood.
Urinary Glucose. Simple office tests or more complicatedquantitative laboratory tests may be used to determine the quantity of glucose lost in the urine. In general, a normal person loses undetectable amounts of glucose, whereas a person with diabetes loses glucose in small to large amounts, in proportion to the severity of disease and the intake of carbohydrates.
Fasting Blood Glucose and Insulin Levels. The fasting bloodglucose level in the early morning is normally 80 to 90 mg/100 ml, and 110 mg/100 ml is considered to be the upper limit of normal. A fasting blood glucose level above this value often indicates diabetes mellitus or a least marked insulin resistance.
In type I diabetes, plasma insulin levels are very low or undetectable during fasting and even after a meal. In type II diabetes, plasma insulin concentration may be severalfold higher than normal and usually increases to a greater extent after ingestion of a standard glucose load during a glucose tolerance test (see the next paragraph).
Glucose Tolerance Test. As demonstrated by the bottomcurve in Figure 78–12, called a “glucose tolerance curve,” when a normal, fasting person ingests 1 gram of glucose per kilogram of body weight, the blood glucose level rises from about 90 mg/100 ml to 120 to 140 mg/100 ml and falls back to below normal in about 2 hours.
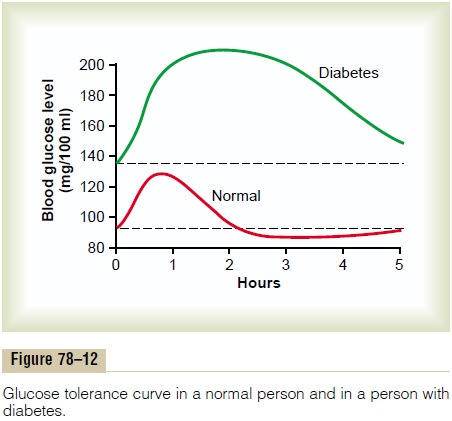
In a person with diabetes, the fasting blood glucose concentration is almost always above 110 mg/100 ml and often above 140 mg/100 ml. Also, the glucose toler-ance test is almost always abnormal. On ingestion of glucose, these people exhibit a much greater than normal rise in blood glucose level, as demonstrated by the upper curve in Figure 78–12, and the glucose level falls back to the control value only after 4 to 6 hours; furthermore, it fails to fall below the control level. The slow fall of this curve and its failure to fall below the control level demonstrate that either (1) the normal increase in insulin secretion after glucose ingestion does not occur or (2) there is decreased sensitivity to insulin. A diagnosis of diabetes mellitus can usually be estab-lished on the basis of such a curve, and type I and type II diabetes can be distinguished from each other by measurements of plasma insulin, with plasma insulin being low or undetectable in type I diabetes and increased in type II diabetes.
Acetone Breath. As pointed out, small quantities of acetoacetic acid in the blood, which increase greatly in severe diabetes, are converted to acetone. This is volatile and vaporized into the expired air. Consequently, one can frequently make a diagnosis of type I diabetes mellitus simply by smelling acetone on the breath of a patient. Also, keto acids can be detected by chemical means in the urine, and their quantitation aids in determining the severity of the dia-betes. In the early stages of type II diabetes, however, keto acids are usually not produced in excess amounts. However, when insulin resistance becomes very severe and there is greatly increased utilization of fats for energy, keto acids are then produced in persons with type II diabetes.
Related Topics