Chapter: Essentials of Psychiatry: Treatment of Violent Behavior
Treatment of Violent Behavior: Long-term Treatment
Long-term
Treatment
The
treatment goal is to decrease the frequency and intensity of aggressive
behavior. Specialized units such as secure or psychiat-ric intensive care units
(Musisi et al., 1989; Goldney et al., 1985; Warneke, 1986; Citrome et al., 1995) provide a structured
envi-ronment that optimizes staff and patient safety. In general these
specialized units are staffed with persons trained in interacting with volatile
and difficult to manage patients (Maier et
al., 1987). When available, these units can be a valuable resource for
educa-tion, training, consultation and referral.
Although
pharmacotherapy remains a mainstay of treat-ment for the persistently
aggressive patient, behavioral plans need to be used in tandem. Providing
structure, including the use of behavioral contracts, can be useful. Preventive
aggression devices (PADS) are a form of ambulatory restraints, which can be
used as an alternative to seclusion (Van Rybroek et al., 1987). The technique was first developed for a specialized
inpatient unit
with
repetitively aggressive patients. Patients in these wrist-to-belt and/or
ankle–ankle restraints can remain with their peers on the ward, eat their meals
and interact, yet are prevented from striking out and injuring others. In combination
with a compre-hensive behavior modification program, these patients can be
weaned off the use of the ambulatory restraints.
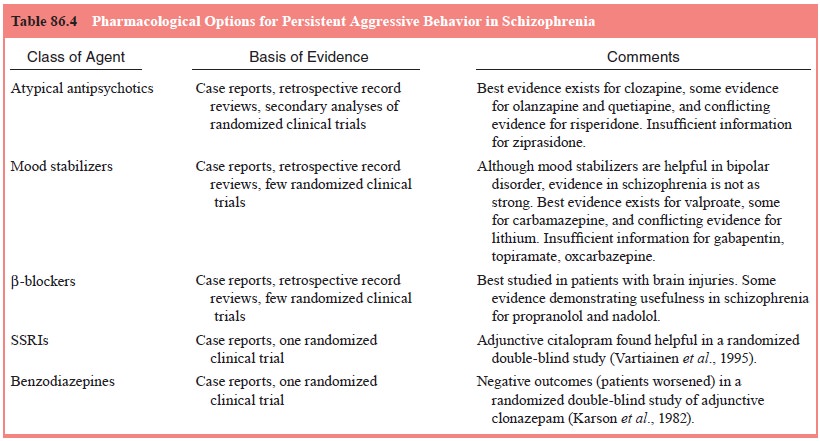
Although
pharmacotherapy for the longer-term man-agement of aggressive behavior is
somewhat dependent on the patient’s underlying diagnosis, clinical management
is often complicated and can entail the use of several coprescribed
medi-cations. At the core of impulsive aggressive behavior may be a
dysregulation of the serotonergic neurotransmitter system and this may explain
the possible ameliorative effects of atypical anti-psychotics and the selective
serotonin reuptake inhibitors (SSRIs). In addition, beta-blockers and
moodstabilizers have been used with some success. Table 86.4 outlines the
medication strategies useful in patients with aggressive behavior and
schizophrenia. Nonadherence to a treatment regimen may require the use of
out-patient commitment, now available in many jurisdictions.
Atypical Antipsychotics
The availability of atypical antipsychotics has led to the observa-tion that these agents may act differently from the older antipsy-chotics in that they may specifically target aggressive behavior. Several retrospective studies have demonstrated a decrease in the number of violent episodes and/or a decrease in the use of se-clusion or restraint among inpatients after they began clozapine treatment (Wilson and Claussen, 1995; Ratey et al., 1993; Chiles et al., 1994; Mallya et al., 1992; Spivak et al., 1997; Maier, 1992; Ebrahim et al., 1994). At this time, the weight of the evidence favors clozapine as specific antiaggressive treatment for schizo-phrenia patients (Glazer and Dickson, 1998), with demonstrated superiority to haloperidol and risperidone (Citrome et al., 2001). More research is needed to compare the other atypical antipsy-chotics with clozapine for this indication. Ideally, such studies need to be done double-blind with subjects specially selected because of their aggressive behavior. This is operationally quite diffi cult because of a number of logistical factors, including the relative rarity of aggressive events and consequent need for a large sample size and lengthy baseline and trial periods, as well as selection/consent bias (Volavka and Citrome, 1999).
Mood Stabilizers
There is
an expectation that adjunctive mood stabilizers can reduce aggressive and
impulsive behavior (Citrome, 1995). This is understandable when the primary
diagnosis is bipolar or schizoaffective disorder where the mood stabilizer is
treating the core symptoms of the disorder, but these agents, notably
valproate, lithium and carbamazepine, are also used, though less frequently, in
patients with schizophrenia.
Beta-blockers
Beta-adrenergic
blockers, in particular propranolol, have been used in the treatment of
aggressive behavior in brain injured patients (Yudofsky et al., 1981, 1984).
Propranolol has also been used as an adjunctive treatment for schizophrenia,
and a reduction in symptoms, including aggression, was found (Sheppard, 1979).
Nadolol may also be helpful (Ratey et al., 1992; Alpert et al., 1990; Allan et
al., 1996). Beta-blockers may exert some of
their effects by decreasing akathisia, which in turn may decrease agitation.
Benzodiazepines
Clonazepam,
a high potency benzodiazepine, had been reported useful in patients with
bipolar disorder. This result is in contrast
to a double-blind placebo-controlled trial of adjunctive clonazepam in
13 schizophrenic patients receiving antipsychotics (Karson et al., 1982). In that study no
additional therapeutic benefit was observed and, in fact, four patients
demonstrated violent behavior during the course of clonazepam treatment.
Using
lorazepam for long-term management (in contrast to acute use as a “prn”) can be
problematic because of physiological tolerance. Missing scheduled doses of
lorazepam may result in withdrawal symptoms that can lead to agitation or
excitement, as well as irritability and a greater risk for aggressive behavior.
Antidepressants
The
current interest in certain antidepressants’ role in aggression is based on the
crucial role of serotonergic regulation of impulsive aggression against self
and others. A number of reports have emerged that posit a role for fluoxetine
(Goldman and Janecek, 1990), citalopram (Vartiainen et al., 1995) and fluvoxamine (Silver and Kushnir, 1998) in the
treatment of persistent aggressive behavior.
Adjunctive Electroconvulsive Therapy
Although
not often considered as a first-line treatment, adjunctive electroconvulsive
therapy (ECT) may be helpful in patients who have inadequately-responsive
psychotic symptoms (Fink and Sackeim, 1996). An open trial of ECT in
combination with risperidone in male patients with schizophrenia and aggression
resulted in a reduction in aggressive behavior for nine of the 10 patients
(Hirose et al., 2001). The
combination of ECT and clozapine may also be helpful. A review of 36 reported
cases treated with this combination, all of whom with a history of
treatment-resistance, revealed that approximately two-thirds benefited from
this treatment (Kupchik et al.,
2000).
Related Topics