Chapter: Essentials of Psychiatry: Treatment of Violent Behavior
Pathophysiology of Aggressive Behavior
Pathophysiology
of Aggressive Behavior
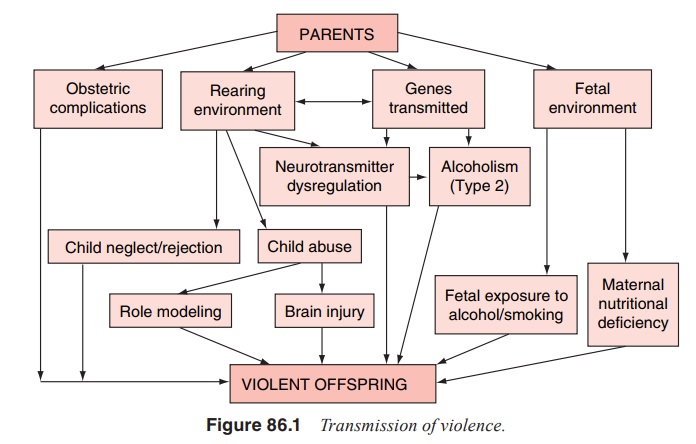
Several
principal pathways leading to a predisposition to aggres-sive behavior are
schematically displayed in Figure 86.1. The par-ents may contribute to the
offspring’s predisposition via transmit-ted genes, fetal environment, obstetric
complications and rearing environment. Several polymorphisms of genes that
control the activity of various neurotransmitters (particularly serotonin and
catecholamines) are apparently associated with persistent aggressive behavior.
Maternal use of alcohol, smoking and malnu-trition during pregnancy were all
reported to explain statistically significant (but clinically modest)
proportions of the variance of aggressive behavior in adult offspring.
Obstetric complica-tions, particularly in interaction with other factors such
as early maternal rejection, may lead to elevated rates of violent crime in the
offspring. Rearing environment not just limited to overt child abuse is one of
the most important factors in the development of predisposition to violence.
Detailed explanation of Figure 86.1, as well as the bibliography supporting it,
are presented elsewhere (Volavka, 2002).
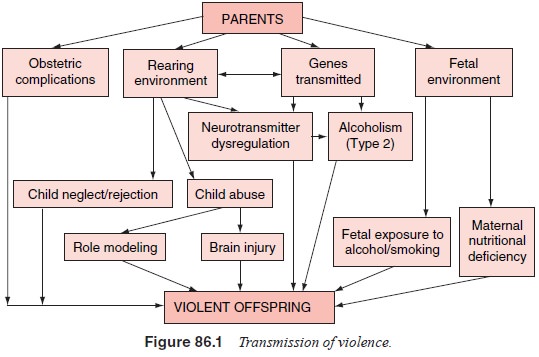
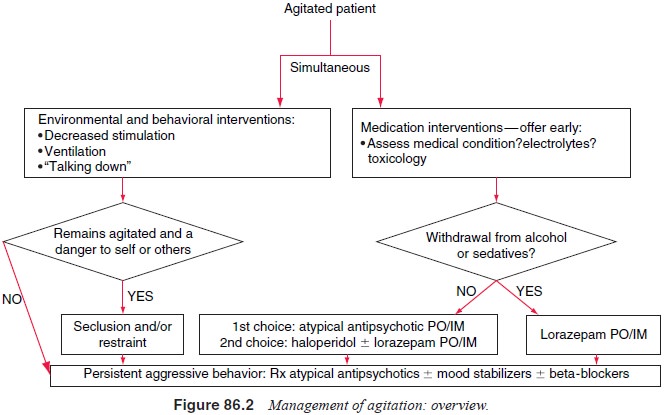
Mechanisms
displayed in Figure 86.2 may operate in per-sons with or without a diagnosable
mental disorder. We will now focus on aggressive behavior in persons with
mental disorders.
Substance Use Disorders
Acute
effects of alcohol and illicit drugs are involved, perhaps causally, in a large
proportion of aggressive incidents. For ex-ample, 51.6% of women injured during
a physical assault by a male partner reported that the assaulter had been
drinking just before the incident (Kyriacou et
al., 1999). Positive urine tests for illicit drugs were obtained in a
majority of arrested males in the USA. Epidemiological stud-ies indicate that
substance use disorders elevate substantially the prevalence of overt physical
aggression (Swanson, 1994).
Psychoses
Most
persons diagnosed with a psychosis are not violent. Never-theless, psychoses
are associated with an elevated risk for aggres-sion. It is clear that
comorbidity of psychosis and substance use disorder contributes to this risk
very substantially. Furthermore, persons with psychoses are more likely to have
substance use dis-orders than other people (Regier et al., 1990). Combination of sub-stance abuse and nonadherence to
treatment is the typical prelude to the development of aggressive behavior in
persons with severe mental illness living in the community (Swartz et al., 1998).
As every
hospital psychiatrist knows, there are many psy-chotic inpatients who are
aggressive without access to alcohol and drugs, and in spite of supervised
antipsychotic treatment. Thus, factors other than substance use and
nonadherence to treat-ment must be involved in the pathophysiology of
aggression in these patients.
From the
standpoint of practical management of aggres-sive patients with major mental
disorders, it seems that it could be fruitful to study in detail individual
assaults in order to assess underlying pathophysiology. This is a promising
avenue of re-search since it is generally agreed that aggressive behavior has
multiple causes that differ among patients, and perhaps among different
incidents in individual patients. Our experience, based on interviews of
assailants, victims and witnesses, as well as on observations of videotapes,
suggests that most assaults among psychiatric inpatients diagnosed with
psychoses are not driven by psychotic symptoms. It appears that many of these
assaults are attributable to comorbid personality disorders.
Personality Disorders
Antisocial
personality disorder (APD) is partly defined by aggres-sive behavior and
therefore it is not surprising that many violent psychotic patients meet its
diagnostic criteria. This circularity of definition makes the use of this
diagnosis somewhat unhelpful. The concept of “psychopathy”, introduced to
modern psychiatry by Cleckley (1976), is less circular since it relies
primarily on personality and psychological processes rather than on criminal or
aggressive behavior. Psychopathy is assessed by a valid and reliable checklist
constructed by Hare and his coworkers (Hart et
al., 1992). Table 86.1 shows the screening version of the check-list
intended for use in persons with serious mental illness (Hare, 1996; Hart et al., 1995). The first six items in Factor-1
measure the severity of interpersonal and affective symptoms of psychop-
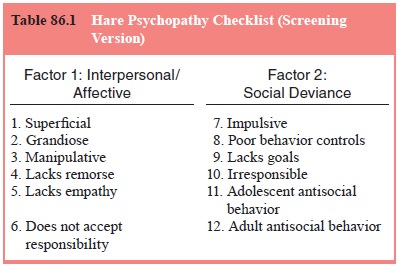
athy. The
next six items in Factor-2 reflect the social deviance symptoms. Psychopathy is
a narrower concept than APD. Most psychopaths meet the criteria for APD, but
subjects diagnosed as APD do not necessarily meet the criteria for psychopathy.
Psy-chopathy predicts violent behavior in nonpsychotic individuals (Hare and
Hart, 1993), as well as in persons with major mental disorders (Hart et al., 1994). The rates of comorbidity
of psy-chopathy and schizophrenia are elevated among violent patients (Nolan et al., 1999).
Differentiating
aggressive behavior based on psychopa-thy from that based on psychotic symptoms
has consequences for treatment. It is unlikely that psychopathy will respond to
antipsychotics.
Related Topics