Chapter: Essentials of Psychiatry: Treatment of Violent Behavior
Acute Agitation
Acute
Agitation
Agitation
can be defined as excessive motor or verbal activity. Common examples include
hyperactivity, verbal abuse, and threatening gestures and language. Unmanaged
acute agitation can lead to violence. As such, acute agitation is a psychiatric
emergency that requires rapid intervention. Oral medication treatment may be
impractical or impossible. This section will focus on intramuscular medications
within the context of a behavioral management plan.
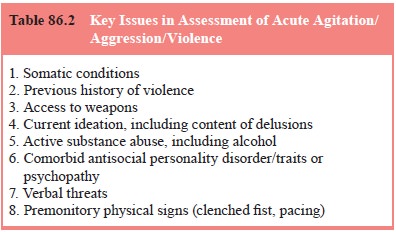
Assessment
Key
points in assessment are outlined in Table 86.2. The time available for patient
assessment will be dependent on the acu-ity of the presentation. For someone
who is acutely agitated and an immediate danger to self or others, emergency
mea-sures must be taken to avoid harm. Somatic conditions must be ruled out
prior to initiating additional treatment, as an underlying metabolic, toxic,
infectious, or other nonpsychiat-ric cause may need to be treated. In these
cases the agitation is a symptom to be treated alongside the underlying
condi-tion. This is not as great a concern for the physically healthy
psychiatric patient whose history is well known to the staff than for the
relatively unknown patient presenting to the emer-gency room. In addition, in
the nursing home environment, new-onset agitation may indicate a newly emerging
somatic condition. Once the patient is under behavioral control further medical
and psychiatric work-ups can be done. Mechanical re-straints may be necessary
to prevent the agitated patient from injuring himself/herself, or others, while
the medical work-up is being conducted.
Care must
be taken not to miss comorbid conditions of alcohol or sedative abuse or
dependence that may present with acute intoxication or withdrawal. Such
conditions will drive the treatment choice towards the use of a benzodiazepine
(see later).
Assessment
should also include the context of the agita-tion. Patients may be purposefully
using aggressive behavior to intimidate others. Antisocial personality traits
may be the most important factor in some instances of patient violence where
goal-directed behavior such as extortion of money or cigarettes is present.
These antisocial behaviors may not always be evident to staff, as they can
occur in unsupervised areas such as hallways, bedrooms and bathrooms. Such
predatory behavior may involve victims who are unable to articulate what is
happening to them, while the aggressor appears to have an abundance of material
goods or undue influence on others.
Where
aggressive behavior may appear to be impulsive or random, environmental factors
may be a significant factor. Some patients are transiently violent when in a chaotic
environment, others are persistently violent no matter the milieu (Krakowski
and Czobor, 1997). In contrast to the persistently violent patient, those who
were transiently violent were more likely to respond to a new structured
environment (Krakowski et al., 1988).
Envi-ronmental factors leading to increased aggressive behavior on a
psychiatric ward include crowding (Palmstierna et al., 1991; Ng et al.,
2001). It appears that the transiently violent are more re-sponsive to typical
antipsychotic medication and have less neuro-logical impairment than the
persistently violent patient (Volavka and Krakowski 1989).
It is
generally agreed that it is impossible to predict with ab-solute certainty if a
violent act will occur, but it is possible to assess risks. Past history of
violence may be the best predictor of future violent behavior (Blomhoff et al., 1990; Convit et al., 1988; Karson and Bigelow, 1987),
and obtaining a history of this, access to weap-ons, and current ideation are
essential elements in risk assessment.
Treatment
Behavioral,
psychological, and pharmacological interventions are used simultaneously
(Citrome and Green, 1990). Clini-cians are urged to survey the environment for
potential weap-ons, not to turn their back on the patient, and to have other
staff available. Taking verbal threats seriously and being aware of physical
premonitory signs such as a clenched fist and pacing are important. Initially,
an agitated patient should be isolated from other patients and from
distractions because extraneous stimulation can intensify psychosis in a
patient who may be hal-lucinating, paranoid and agitated. Moreover, other
patients may intentionally or inadvertently interfere with treatment. Generally
it is easier to clear the area of many calm patients than to move one dangerous
individual. Restraint or seclusion may be neces-sary, and this is the time
where the risk for injury for both staff and patients is highest. The technique
of the calming blanket, a soft comforter with canvas reinforcements, may be
helpful in subduing the patient who is punching, scratching, or kicking.
Psychotherapeutic Approaches
Nonspecific
sedation is often used in the management of an acutely agitated patient. In
general, intramuscular injection of a sedative has a faster onset of action
than oral administration but it has been observed that a patient may calm down
readily after an oral dose, knowing that action has been taken and help is
being provided. Previously, choice of intramuscular medication for these
behavioral emergencies has been limited to typical antipsy-chotics (such as
haloperidol or chlorpromazine) versus benzodi-azepines (principally lorazepam)
(Table 86.3). The availability of intramuscular formulations of novel atypical
antipsychotics pro-vides additional treatment options for the management of
acute agitation in patients with psychosis (Citrome, 2002). Lorazepam, the only
benzodiazepine that is reliably absorbed when adminis-tered intramuscularly,
appears to be a good rational choice when treating an acute episode of
agitation, especially where the etiol-ogy is not clear such as when a patient
with a history of schizo-phrenia may actually be withdrawing from alcohol
(Salzman, 1988; Greenblatt et al.,
1979, 1982). Caution is required when respiratory depression is a possibility.
There may be increased risk of this in patients with sleep apnea (associated
with being morbidly obese, history of snoring and daytime drowsiness).
Lorazepam is not recommended for long-term daily use be-cause of the problems
associated with tolerance, dependence and withdrawal. Paradoxical reactions to
benzodiazepines, as exhib-ited by hostility or violence has been an area of
concern (Bond and Lader, 1979), but the evidence is not convincing and, in any
event, such reactions are uncommon (Dietch and Jennings, 1988). The possibility
of alcohol or sedative withdrawal as a cause of agitation is another point in
favor of using lorazepam.
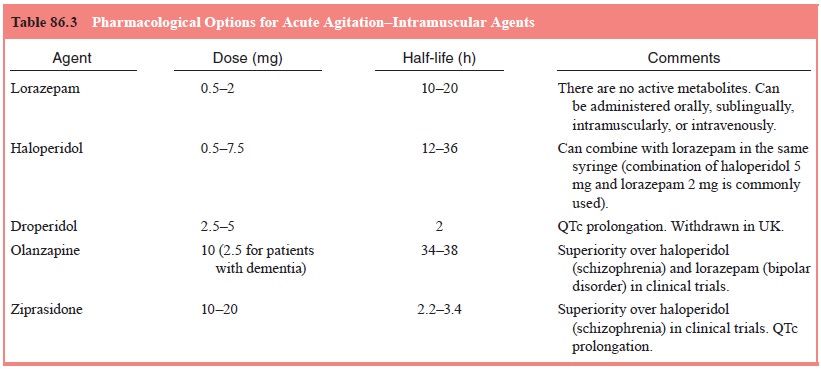
The
typical antipsychotics cause sedation, given in a high enough dose.
Haloperidol, a high potency butyrophenone, has been frequently used as an
intramuscular prn medication for agitation and aggressive behavior in an
emergency department setting for a wide variety of patients (Clinton et al., 1987). De-pending on the
clinical response, subsequent doses may be ad-ministered as often as every hour
if necessary. However, 4- to 8-hour intervals may be satisfactory.
Haloperidol’s advantage over the low potency typical antipsychotics (e.g.,
chlorpromazine) is that it causes less hypotension, fewer anticholinergic side
effects, and causes less of a decrease in the seizure threshold. In addition to
this nonspecific sedation, a benefit would be its antipsychotic effect (in
responsive patients), but this would be evident only after the acute episode of
agitation has subsided. High doses of typical antipsychotics may lead to more
adverse effects, includ-ing akathisia, which may itself provoke violent
behavior (Keck-ich, 1978; Siris, 1985).
The new
atypical antipsychotics may emerge as important options in the management of
acute agitation in schizophrenia. Although sedation or “calming” remains the
primary mode of action when used emergently in the acutely agitated patient,
the atypical antipsychotics have several advantages over typical
an-tipsychotics (Citrome, 1997), in particular a lower propensity for
extrapyramidal side effects, including akathisia.
Related Topics