Chapter: Essentials of Psychiatry: Combined Therapies: Psychotherapy and Pharmacotherapy
Combined Therapies: Psychotherapy and Pharmacotherapy
Combined Therapies: Psychotherapy
and Pharmacotherapy
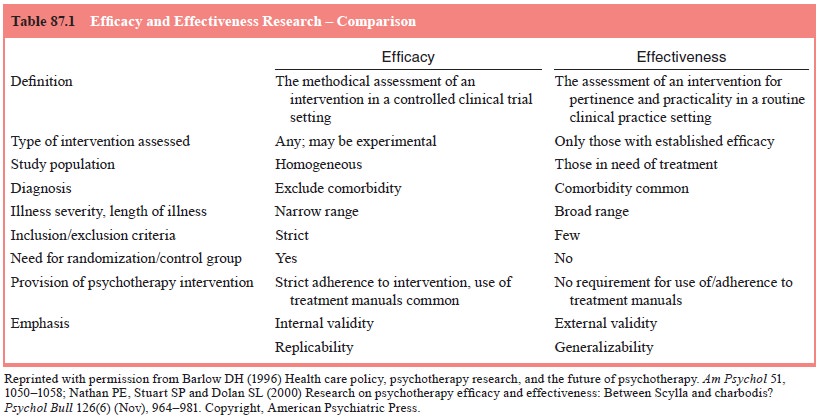
The
rationale for combining treatment modalities is based on the idea that the
strengths of each modality are promoted while the weaknesses are minimized,
producing results that are better than with either modality alone (Hollon and
Fawcett, 1995). Although intuitively this rings true, psychiatrists have a duty
to incorporate evidence-based approaches into their clinical practice. While
most evidence-based mental health research in the literature is based on
efficacy studies, there has been a recent move towards conducting effectiveness
studies that are hoped to be of increased relevance to general outpatient
clinical practice (Nathan et al.,
2000). Table 87.1 highlights the differences between efficacy and effectiveness
research (Barlow, 1996; Nathan et al.,
2000). Re-cent literature examining the efficacies of combined treatment (not
necessarily integrated treatment by a psychiatrist) vary by disorder, timing of
treatments and whether administered during the acute or maintenance phase.
Recent literature has also exam-ined the sequential application of combined
treatment (Fava et al., 2001; Frank et al., 2000). Effectiveness studies are
far fewer, as mentioned, and do not always demonstrate superiority of com-bined
approaches over either medication or therapy alone.
Hollon
and Fawcett (1995) have outlined four ways in which combined treatment may
prove advantageous over either treatment alone: increase the magnitude,
probability, or breadth of clinical response, and increase the acceptability to
the patient of either modality. In general, they feel that there is literature
to support the statement that combined treatment enhances the breadth of
clinical response. It is within this context that clini-cal practice guidelines
published by the Agency for Health Care Policy and Research support the use of
combined treatment in depressive disorders (Depression Guideline Panel, 1993).
Various
authors discuss the potential benefits of employ-ing pharmacotherapy within a
psychotherapeutic context (Kler-man, 1991; Kay, 2001). Pharmacotherapy has been
noted to have a quicker onset of action on acute symptoms than most
psycho-therapies, perhaps with the exclusion of cognitive therapy (Hol-lon and
Fawcett, 2001). It is felt that this rapid dampening of symptoms may enhance
the patient’s ability to more productively participate in therapy by a variety
of mechanisms. These have been described cogently by Klerman (1985, 1991) and
include en-hancing the patient’s self-esteem, creating a safe environment in
which emotions are more freely discussed, reducing the stigma of seeking mental
health care through a positive placebo effect, im-proving cognition
(verbalization and abreaction), and functioning as a transitional object during
breaks in therapy, among others.
The
benefits of employing psychotherapy within a primarily psychopharmacologic
relationship have also been described. Empirical evidence exists across the
spectrum of mental health disorders to support the following suggested benefits
of adding psychotherapy to medications. It decreases the incidence of illness
relapse (Hogarty et al., 1986), as
well as symptom relapse upon medication discontinuation (Wiborg and Dahl, 1996;
Spiegel et al., 1994). It fosters the
patient’s ability to utilize healthy coping
strategies, addresses issues that are not typically targeted by
psychopharmacologic treatment such as dysfunctional relationship patterns or
negative self-appraisals due to traumatic past events, and enhances
psychotropic compliance (Paykel, 1995; Cochran, 1984).
Clinical Applications: Treatment Adherence
Adherence
may be enhanced in part through discussion of the patient’s metaphor for the
medication, either positive or negative (Kay, 2001).
The above
case highlights one of the beliefs that patients may have regarding
medications, that is, they indicate their provider’s level of interest in them
as a person and the provider truly appreciates the level of their distress. In
certain contexts these beliefs may be regarded as a “positive metaphor”;
however in others, as demonstrated above, it may hinder the patient’s response
to treatment, their compliance with the treatment regimen, and their level of
trust in their provider.
Clinical Applications: Sequential Treatment
Fava (1999) highlights that sequential treatments may be applied in four ways: 1) using a second type of psychotherapy when the first orientation has not fully achieved treatment goals; 2) introducing a second type of pharmacotherapy when the first medication has not achieved adequate symptom relief; 3) introducing psychotherapy when initial pharmacotherapy has not been fully effective; and 4) introducing pharmacotherapy when initial psychotherapy has not been fully effective. The latter two may include use of combined treatments in a sequential fashion.
As
demonstrated by the vignettes, the meanings that the patient attributes to
medication may have to do with cognitions and feelings in a variety of spheres
including the illness, the pro-vider, and themselves (Beck, 2001).
Clinical Applications: Advantages and Challenges
The
vignettes also serve to highlight potential benefits and chal-lenges
surrounding integrated treatment described by Kay (2001). Integrated treatment
essentially eliminates the communication difficulties encountered in split
treatment set-tings. The practitioner of integrated treatment does face some
obstacles. In both cases, the psychiatrist needs to be well trained in a
variety of psychotherapy orientations, particularly in the orienta-tion that
has evidence to support its use in a particular disorder.
To
provide a theoretical framework for formulation of the patient and treatment
plan, McHugh and Slavney (1983) similarly discuss understanding the
psychiatrically ill patient from four “perspectives”. These multifactorial
models of mental health illnesses serve as conceptual tools with which to
understand the whole patient and those forces that together precipitate,
perpetuate and modify illness course/progression. It stands to reason that a
provider of integrated care should utilize an “integrated” model of illness
description, etiology and treatment.
When a
single provider directs both forms of treatment, traditional role conflicts may
emerge. The role stereotype of a psychotherapist may include one who has a
multidimensional understanding of the patient, is interested in
intrapsychic/core conflicts and their manifestations in symptoms, behaviors,
feel-ings and thoughts, and whose style is less authoritarian. The
pharmacotherapist’s traditional role stereotype is of a biological/
neurochemical understanding of the patient and a prescriptive, structured, more
authoritarian style in approaching diagnosis, medications and other issues.
While these roles are, as described, stereotypic, they do have in common the
role of the provider in establishing rapport and a therapeutic alliance with
the patient. It has been suggested that the psychiatrist who uses an integrated
model provides more time for development of the therapeutic al-liance thus
increasing the patient’s comfort in disclosing embar-rassing side effects of
medication and, perhaps, even aiding in treatment outcome via the strength of
the alliance (Gabbard and Kay, 2001). Psychotherapy studies have suggested that
therapist variables accounted for 30% of the variance in outcomes, and that
therapeutic alliance is perhaps the most important factor in positive treatment
outcomes (Lambert, 1992; Svartberg et al.,
1998). The therapeutic alliance is crucial; as such, management of transitions
between roles, as well as the seamless integration of roles is imperative
within the practice of integrated treatment (Gabbard and Kay, 2001). These role
transitions may occur rap-idly and within a single session.
A
familiarity with current literature and clinical practice guidelines concerning
when to employ medications alone, ther-apy alone, or both, and when sequential
treatments may lead to a greater probability of remission is a must for any
clinician utiliz-ing combined treatment.
Clinical Applications: Managing the Session
This
example highlights one way in which to fluidly incorporate both domains
(psychotherapy and pharmacotherapy) within each patient visit. The above
approach is structured in nature, follow-ing cognitive therapy’s principle that
sessions are structured and remain constant during therapy (Beck, 1995).
Providers of psychodynamic therapy, among other types of therapy, often prefer
this structured type of approach, advocating that medica-tion use either be
discussed at the beginning or at the end of the session. Proponents of the
beginning method feel that discussion of medication issues ensures adequate
time is spent on concerns and may provide important material for the session.
Advocates of the “set aside 5 to 10 minutes at the end of the session” ap-proach
feel that it is most important for the patients to set their own agenda, as
this allows for time needed for the patient to regain composure/recompensate
before the end of the session. Another approach is the nonstructured method. In
this case the therapist addresses medication issues only when the need arises.
As there are no evidence-based studies to guide clini-cal practice, it is most
important to base the choice on patient and provider preference and to practice
consistency with each patient (Kay, 2002).
Clinical Applications: Individualizing Treatment
How can
the psychiatrist tailor his/her treatment options to each individual patient?
When would sequential approaches be indicated and in which disorders are
combined treatments most likely to be helpful? During which phase of treatment
(acute versus maintenance) should combined treatments be used versus solo
treatments (either medications or therapy)? For what severity of illness are
combined treatments pre-ferred? Is there evidence to support sequential
approaches and should they be specifically targeted to stages of the illness?
How might understanding physiologic changes in the brain, which occur in the
context of both medications and psycho-therapy, help guide our research and
clinical treatment inter-ventions? It should be kept in mind that research regarding
these issues is in its infancy, and many recommendations may require further
studies definitively to aid with the establish-ment of critical pathways for
each of the disorders In spite of the need for further research, combined
treatment appears useful for all major categories of psychotic illness,
including anxiety and mood disorders, psychotic disorders, eating disor-ders
and substance abuse.
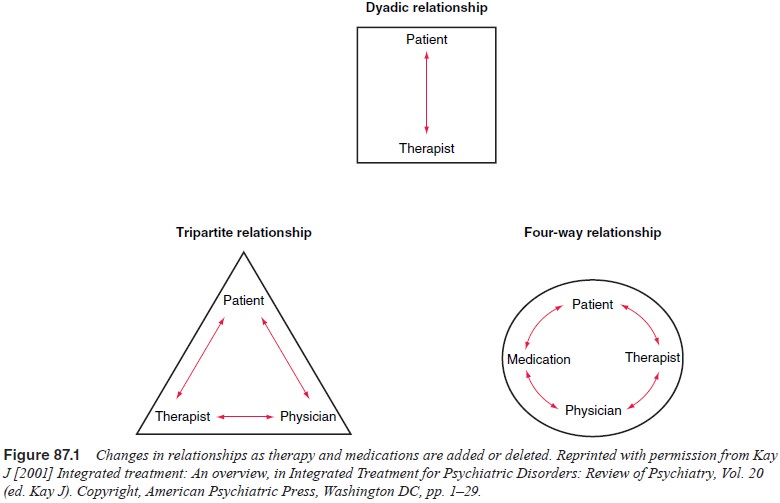
Split Treatment
The last
few decades have seen an increasing shift from a single relationship between patient
and psychiatrist towards a tripartite relationship with the inclusion of
medication, or to a four-way or systemic relationship with the addition or
deletion of medications (Figure 87.1). Thus, combined treatments are commonly
provided by two or more clinicians, hence the term “split”.
Related Topics