Chapter: Essentials of Psychiatry: Combined Therapies: Psychotherapy and Pharmacotherapy
Toward Successful Split Treatment
Toward
Successful Split Treatment
The
following suggestions are offered as organizing principles for these three
stages (with permission from American Psychiatric Press, Riba and Balon, 2001):
A key
aspect of split treatment is how complex and dif-ficult such treatment is for
the clinicians, the patient and the pa-tient’s family. Unless one works in a
clinic or organized setting where relationships between clinicians are
well-delineated (e.g., one psychiatrist works with a specific group of
nonmedical thera-pists), much thought must go into managing safe and effective
split treatment.
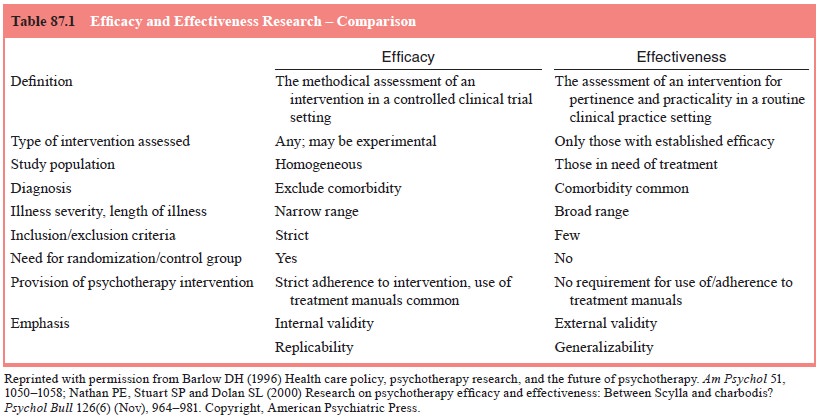
It may be
helpful to think of split therapy having a begin-ning, middle course, and end
(Table 87.1). In order to avoid or minimize the pitfalls associated with split
treatment, the follow-ing clinical suggestions are provided as organizing
principles for its three stages (Rand, 1999; Tasman and Riba, 2000):
Beginning of Treatment
·
Communication is key to providing excellent care in
split treatment. At the beginning, both clinicians should obtain a signed
release-of-information form from the patient. Commu-nication must be regular
and frequent between the clinicians and the patient should be made aware of
these discussions. The forms of regular communication should be decided at the
onset – routine telephone calls, faxes, emails, follow-up letters and the like.
The patient should not be a messenger between the clinicians.
·
Issues of confidentiality should be discussed and
reviewed at the beginning of treatment. Confidentiality should not be used as a
cover to hide from taking the time to make telephone calls, to send copies of
evaluations and follow-up notes, to send emails or faxes, or to have joint
sessions with both clini-cians and the patient.
·
Diagnostic impressions should be independently
arrived at, then discussed and agreed upon. If there is a difference of
opinion, an understanding must be reached before treatment proceeds.
·
The clinicians must work with each other and with
the patient to determine the treatment plan. The treatment plan should specify
how often each of the clinicians expects to see the pa-tient and what process
to pursue if the patient does not follow-up or if there is a missed
appointment. If the patient wishes to end either the therapy, the medications,
or both, it has to be un-derstood that all parties will discuss this important
decision. It is desirable for a written contract to be drawn up between the
clinicians and the patient so that all parties understand what the agreement
for services will entail. Included in the contract should be a delineation of
the clinicians’ roles and responsi-bilities, as well as those of the patient.
·
Clinicians vacation schedules and other on-call and
cover-age issues must be discussed regularly and documented. The patient needs
to know whom to call in an emergency. At the beginning of split treatment, both
clinicians and the patient should be aware of their respective beliefs
regarding medica-tion and psychotherapy.
·
There must be a discussion about what type of care
would be optimal for the patient and if there are barriers to such care. The
patient should be informed of this review; if possible, he or she should
participate in it.
·
The clinicians should discuss their professional
backgrounds and training with each other at the beginning of the patient’s
treatment. Issues such as licensure, ethics, violations, mal-practice claims,
hospital privileges, coverage of professional liability insurance,
participation on managed care panels and commitment to split treatment should
all be made clear.
·
The clinicians need to agree who will communicate
with third parties regarding the patient’s care. Further, each clinician should
know the patient’s mental health benefits and means of payment. There needs to
be an agreement by all parties as to the use of such benefits.
·
The clinicians need to understand how best to
interface with the patient’s family or significant others.
·
If the patient has health providers other than the
psychiatrist and therapist (e.g., primary care physician, cardiologist a
physical therapist), it should be decided which clinician will be the
designated communicator or coordinator with those other providers.
·
At the beginning of treatment there should be a
review of how each clinician will assess and manage the patient’s thoughts
regarding or attempts at suicide, homicide, violence and domestic abuse.
·
It should be made clear to the patient what
symptoms or types of issues should be brought to the attention of which
clinician.
·
It is helpful for the clinicians to decide how
problems will be handled as the need arises.
·
The clinicians should discuss differences in fee
schedules, cancellation policies, length of visits and frequency of visits.
Middle Course
·
Special attention must be paid to transference and
counter-transference in this type of system of care. Disparaging and negative
remarks made by the patient concerning either clini-cian, therapy, or
medication must be understood and managed in the context of this complex type
of treatment.
·
Clinicians should review how many cases of split
treatment they have in their practices and whether or not this is a safe mix.
Factors to consider include the clinical complexity of the cases, how busy the
practice is, the influence of third-party payers and the hassle factor, the
number of different clini-cians one is working with, the psychiatric disorders
of one’s patients, and so on. It may be prudent to determine the risks involved
in having a large patient population in split treatment and to weed the number
of such patients down to an accept-able level. Further, clinicians should
minimize the number of collaborators, since it is virtually impossible to keep
track of a large number of clinicians’ credentials, vacation schedules,
communication patterns, and so on.
·
Adherence to medications and to psychotherapy
should be ad-dressed equally.
·
Treatment plans should be regularly reviewed and
updated be-tween the clinicians and the patient.
·
Use of the patient’s mental health benefits should
be regularly reviewed and discussed between the clinicians and the patient when
appropriate.
·
There must be an agreement that either clinician
can terminate the split therapy but that the patient must be provided adequate
and appropriate warning and referrals to other clinicians. In other words, the
patient cannot be abandoned.
Ending Split Treatment
·
After reviewing the treatment plan, both clinicians
and the pa-tient will decide together on the goals that have been met or have
not been realized and the best time for termination. They should decide how to
stagger the discontinuation of therapy and of medication.
·
It is important to consider how to manage follow-up
and recur-rence of symptoms.
The
clinicians must have a system for giving each other feedback on the care each
is providing to the patient. Ideally, after the treatment is complete, the
clinicians should review any aspects of the case that could have been managed
or handled differently. Ideally, the patient should be part of this evaluation
process as a way of assuring continuous quality improvement. Most importantly,
throughout all stages of the split treatment process, clinicians need to
respect both the patient and each other’s professional understanding.
Although
the challenges of split treatment are great, there are many reasons for
clinicians and patients to try to surmount the obstacles. Good communication
patterns between clinicians and many of the suggestions noted here may be
guideposts on the path toward successful split treatment.
Related Topics