Chapter: Essentials of Psychiatry: Medication Compliance
Medication Compliance
Medication Compliance
Introduction
Compliance,
or the degree to which patients’ behaviors coincide with the recommendations of
health care providers, is an important component in the understanding of
patient outcomes, particularly in light of a growing regimen of efficacious and
expensive medical treatments. There is an evident gap between the efficacy of
regimens tested in tightly controlled clinical trials and their effectiveness
when applied to “real world” patient experiences. One explanation for this
“efficacy-effectiveness gap”, when treatment regimens move from efficacy trials
into everyday practice, is the apparent decline in patient compliance. Other
terms closely related to compliance include “adherence”, “fidelity”, and
“maintenance”.
Compliance
is difficult to quantify for several reasons. Completely attributing the
difference between an expected and observed treatment effect to problems with
medication com-pliance may be overly simplistic. Several other factors such as
differences in population, degree of comorbidity with other psy-chiatric or
medical diagnoses, and severity of illness may all ad-versely affect the
potential benefit to the patient. Poor or partial compliance with treatment may
have a variable effect on treat-ment outcomes depending on the pharmacokinetic
profile of the medication in question. For example, occasional missed doses of
very long half-life medications will alter serum drug levels to a lesser extent
than in short half-life compounds. Therefore, the issue of partial compliance
with treatment regimens may become more critical depending on the specific
regimen.
A Theoretical Construct for Compliance: The Health Beliefs Model
The
health beliefs of individuals play a major role in their deci-sion-making
processes regarding participation in recommended treatment. A framework that
may be useful in understanding the complex nature of compliance with medical
regimens is the health beliefs model (HBM). Derived from social psychological
theories of Kurt Lewin, the HBM is grounded in the phenom-enological
orientation of perception driving action (Rosenstock, 1974). While this model
was originally designed to study the utilization of screening tests for
detection of asymptomatic diseases, it has been adapted to the areas of
medication compli-ance among psychiatric patients (Kelly et al. 1987).
Five
components of the HBM apply directly to issues of patient compliance. Figure
88.1 depicts the relationship between these components and ultimate compliance
with treatment.
Susceptibility:
patients must see themselves as vulnerable to a serious illness.
·
Severity: patients must realize that he/she has an
illness with health consequences that will continue without medical attention.
·
Perceived benefits: patients must recognize that an
effective treatment exists for their condition. Benefits from psycho-tropic
medication treatment may include the understanding that treatment ameliorates
mental problems or helps avoid rehospitalization.
·
Barriers: common barriers to pharmacologic
interventions in-volve access to medication, adequate psychiatric follow-up,
and adverse effects from the medication.
·
Cues to action: lastly, patients must experience an
internal or external motivation or “cue” to engage in the specified action that
may benefit them.
Cues that
may trigger a patient to participate in their medica-tion regimen typically
relate to a return of symptoms attributed to their mental illness such as
anxious, depressive, or psychotic states.
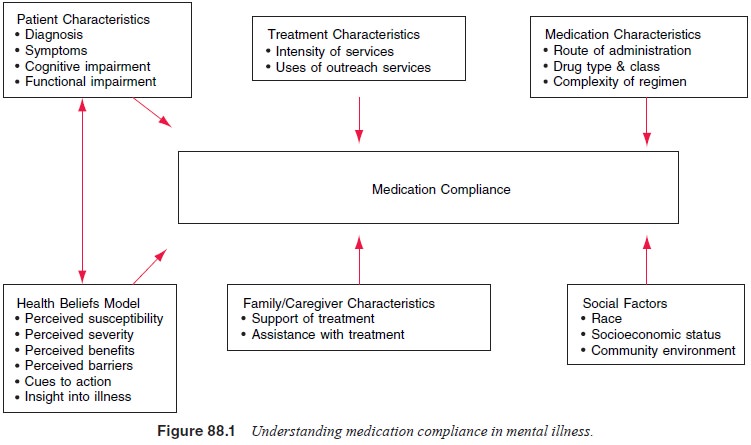
Another Conceptual Model of Compliance
Another
approach to understanding compliance behavior involves the categorization of
problems with compliance along the three domains of psychological problems,
planning problems, and medical problems. These three domains have been used to
develop a compliance checklist as seen in Table 88.1 (Corrigan et al., 1990, Cramer 1991). Psychological
problems include issues such as nonacceptance of
diagnosis or treatment, negative emotional reactions or negative thoughts, and
social criticism from family or friends. Problems
with planning consist of forgetting to take medications, disruption of
usual schedules, and issues with availability of medication. Medical problems that affect compliance include adverse reactions, exacerbation of illness that leads to incapacity to
administer or tolerate medications, or perceptions that medications may lack
efficacy in a given individual. Both HBM and the compliance checklist provide
useful starting points to begin the analysis of problems with compliance in
specific patients or patient populations.
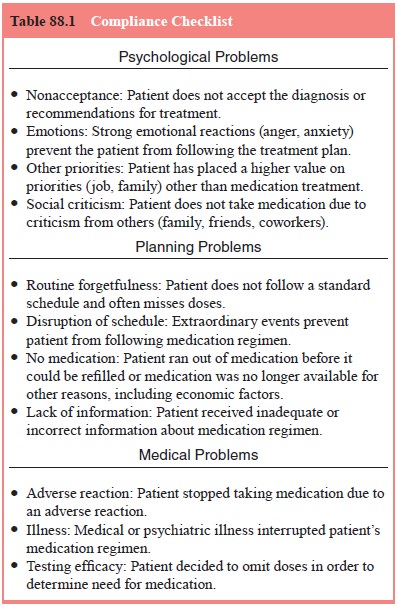
Interventions to Enhance Compliance
General
strategies to enhance compliance take many forms and can be tailored to the
specific needs identified in individual pa-tients. Most approaches to enhance
compliance involve the intro-duction of techniques to improve outpatients’
self-administration of oral medication therapies. Cramer (1991) identifies
several strategies to approach problems with compliance (Table 88.2).
The
action of monitoring compliance itself may improve adherence to proposed
medical regimens, just as frequent weight monitoring may promote weight loss
even without a specific diet regimen. Some data indicate that compliance rates
improve sig-nificantly when outpatients with psychiatric disorders are given
continuous feedback on their medication dosing (Cramer and Rosenheck, 1999).
Compliance-enhancement
interventions that have been studied include individual, group and family
formats and involve diverse theoretical orientations. Unfortunately, many of
the studies that investigate compliance therapies do not also assess the distal
impact on treatment outcomes leaving the clinician unable to evaluate whether
marginal improvements in compliance would in fact lead to cost-effective
improvement in treatment outcomes.
One
intervention referred to as compliance
therapy utilizes a specific approach to individual or group psychotherapy
with cognitive therapy and motivational interviewing techniques (Goldstein,
1992; Hayward et al, 1995).
Therapists attempt to help the patients form a cognitive link between
discontinuation of medication treatment and relapse of symptoms. Using the
patient’s frame of reference, therapists seek to instill a sense of cognitive
dissonance between discontinuation of medication and achievement of the
patient’s own goals. Problem-solving techniques are also employed to identify
internal and external cues that may compromise future medication compliance.
Other
psychosocial interventions to increase compliance in patients with
schizophrenia have also been demonstrated to be effective. Kelly and Scott
(1990) found that strategies aimed at ed-ucation of patients’ families about
compliance and those directed at patients themselves both improved compliance.
No significant difference between the two interventions could be demonstrated.
It is important to note that, given the multiple factors associated with
clinical course, not all improvement in treatment outcomes in schizophrenia is
directly attributable to improved medication compliance. Psychosocial
interventions that lack a specific fo-cus on treatment compliance may
nonetheless have salutatory effects on patient outcomes, regardless of changes
in compliance behavior. Zhang and colleagues (1994) found that family therapy
without a specific focus on compliance produced improvement in relapse rates in
schizophrenic patients independent of changes in medication compliance.
Another
approach to increasing compliance involves the change in route of
administration of medication from oral
preparationsthatmustbetakenatleastoncedailytodepotinjections, such as
haloperidol decanoate and fluphenazine decanoate, that are typically administered
every 2 to 4 weeks. The advantages to depot preparations include supervised
administration of the medication by health care providers, decreased
variability in serum concentrations of the active medication, and no
significant difference in adverse effects as compared with similar oral agents.
Disadvantages include the limited number of medications available in depot
form, the difficulty of scheduling potentially more frequent clinic visits for
injections, and the increased cost
in clinic
staffs’ time with administration of the treatments. At the time of this
publication, no atypical antipsychotic agents were available in depot form.
Therefore, a comparison of compliance with conventional depot agents and
atypical oral agents may be limited in utility. Few studies of depot
antipsychotic preparations address the issues of long-term compliance and
differences in health outcomes when compared with oral agents (Adams and
Eisenbruch, 2002; Quraishi and David, 2002). However, some evidence suggests
that depot antipsychotic agents do confer a marginal improvement in reducing
relapse rates (Glazer and Kane, 1992).
Related Topics