Chapter: Essentials of Psychiatry: Combined Therapies: Psychotherapy and Pharmacotherapy
Negative Aspects
Negative
Aspects
Communication
While
communication is probably the most important factor in successful split
treatment, it is rarely done well (Hansen-Grant and Riba, 1995). Without a
systematic way for clinicians and the patient to have regular, documented
communication, there often arise misunderstandings and misconceptions. Further,
patients are sometimes put in the middle of having to be the messenger between
the clinicians. Needing to communicate puts additional burdens and stress on
busy clinicians with the telephone or in-person time not usually reimbursable.
Poor communication leads to misinter-pretation of what should be attributable
to psychodynamic issues or medication side effects, or both – a poorly
constructed treat-ment plan, ill-defined plans for discharge from treatment,
lack of coordination with family members, neither the clinician nor pa-tient
fully understanding vacation or coverage issues, and so on.
Interdisciplinary Issues
The
literature demonstrates that when clinicians know one an-other, they are more
comfortable with split treatment (Goldberg et
al., 1991; Weiner and Riba, 1997). Unfortunately, often the clinicians do not know one another,
which leads to basic mis-trust, competition, or inequality in the relationship
(Baggs and Schmitt, 1988). Further, this devaluation can be displaced onto the
patient during critical treatment decisions, with certain pa-tients exploiting
this competition even further (Kelly, 1991). The psychotherapy skills of
psychiatrists and nonmedical therapists and the psychopharmacologic education
of social workers and psychologists are all highly variable, contributing to
mistrust (Neal and Calarco, 1999). In such circumstances, the patient may
actually be seen more often by both clinicians and have ill-defined treatment
goals.
Transference and Countertransference
When
patients are referred by their therapists for medication evaluations, the
reactions are variable, but often negative. Such reactions include feeling
abandoned or rejected, as if the therapist has lost interest or given up, like
a failure because therapy did not work, devaluation of the psychotherapy and
the therapist, ideali-zation of the physician, shame, resistance to further
psychody-namic exploration of issues and a narcissistic injury (Busch and
Gould, 1993). Busch and Gould note the difficulties for the thera-pist who
needs to make the referral: shame that help is needed and anger towards the
patient for needing additional help. The psychiatrist could then collude with
the patient’s negative trans-ference towards the therapist and the
psychodynamic process.
Results
of such negative transference could lead to premature closure within the
therapeutic process (Bradley, 1990). There may be a flight into health by the
patient when the medication is first prescribed. The patient and physician may
then realize too late that there was an overreliance on biologic interventions.
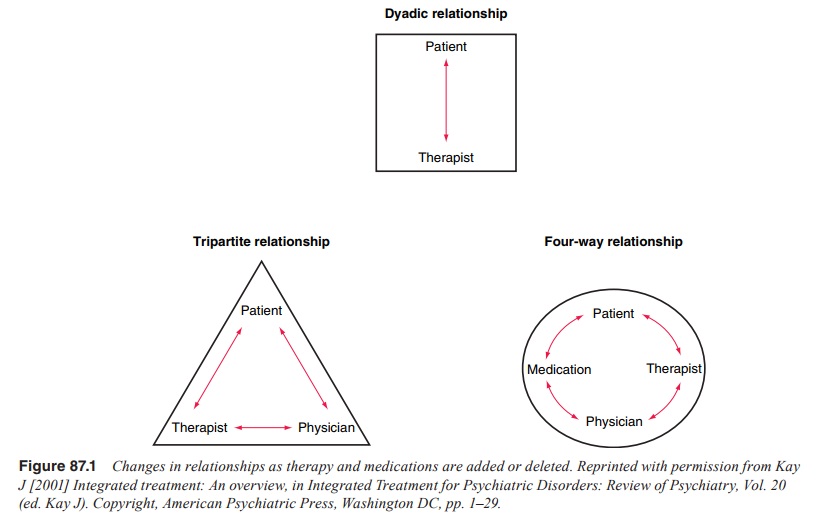
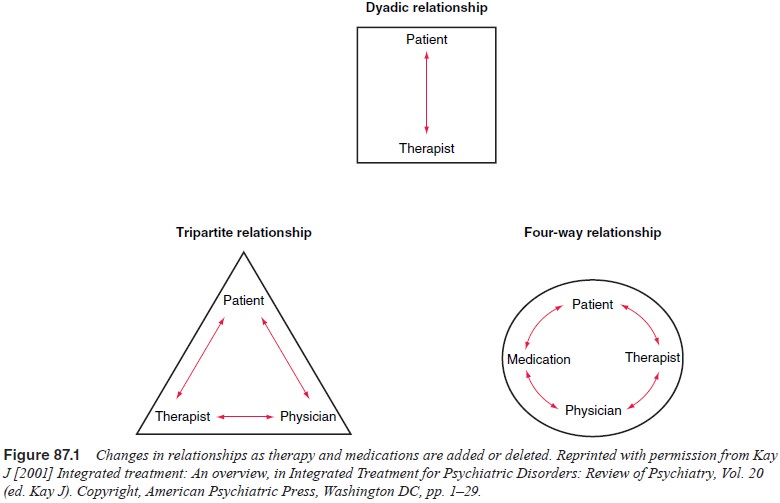
The dyadic relationship between the therapist and patient is changed with the
addition of a physician and medication (see Figure 87.1) leading to distortions
and transference changes in all the relationships.
Related Topics